This is an automatically translated article.
The article is professionally consulted by Master, Doctor Le Thi Minh Huong - Emergency Medicine Doctor - Department of Resuscitation - Emergency - Vinmec Nha Trang International General Hospital. The doctor has more than 06 years of experience in examining and treating internal diseases, emergency and emergency resuscitation.1. What is multiple system atrophy?
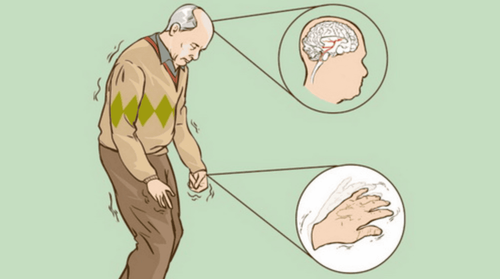
Multisystem atrophy (English name: Mulitple System Astrophy - MSA) is a form of neurodegenerative disease. The disease progresses gradually with symptoms of Parkinson's disease, impaired vegetative function, urogenital dysfunction, cerebellar ataxia and corticospinal tract disease.Multiple system atrophy is also known as Parkinson's - Plus syndrome (Parkinsonism - Plus Syndrome) or atypical Parkinsonian syndromes (Atypical Parkinsonian Syndromes).
Multisystem atrophy is classified into 3 main groups:
MSA - A (Autonomic in Autonomic Nervous System): also known as Shy - Drager syndrome. MSA-P: is Parkinson's disease multisystem atrophy. In addition, the disease is also known as striated black matter degeneration (SND - Striatonigral Degeneration). MSA-C: is cerebellar atrophy (OCPA - Olivopontocerebella Atrophy) or multiple cerebellar system atrophy.

2. Symptoms of multiple system atrophy
Common symptoms in people with multiple system atrophy include:Slow, stiff, or frozen movements. The ability to balance and coordinate movements declines, even disappears. Postural hypotension, especially when standing, significantly reduces blood pressure leading to blurred vision, dizziness, and fainting. Impotence in men Constipation, urination disorder. Difficulty swallowing and speaking.
3. Diagnosis and treatment of multisystem atrophy
3.1 Diagnostic imaging of multisystem atrophy In the diagnosis of multisystem atrophy, one of the frequently used useful tools is MRI imaging. Performing an MRI makes it possible for doctors to distinguish between two forms of multiple system atrophy MSA – C and MSA – P.MSA – C (or OCPA)
MRI scans show typical images of a patient with MSA – C is selective pontine atrophy with flattened lower surface, concurrent pons with Hot Cross Bun Sign and bilateral middle cerebellar peduncle signal (MCP Sign - Middle Cerebella Peduncle) ). The cause of this hyperintensity is the loss of neurons in the pons leading to increased water and gliosis. In addition, the typical MRI images obtained showed atrophy of the middle cerebellar peduncle, pons, worm lobes and inferior bulbar fillings, preserving the roof membrane, superior cerebellar peduncle and pyramidal bundle.

Some diagnostic signs of MSA-P disease are based on MRI images such as putamin atrophy and slit-like void sign caused by hyperintensity on T2-weighted lateral border pallor. The reason for this is increased gliosis and increased water content when the duckweed loses neurons.
In addition, the patient may be ordered to check the nerves, eyes, muscles and blood pressure when changing positions (standing up or lying down).
4. Treatment of multisystem atrophy
Currently, there is no method to completely cure multisystem atrophy, but only to help control the symptoms of the disease. Depending on the condition and severity of each person's disease, the doctor will prescribe different medications.To improve the symptoms of balance disorder, muscle stiffness and slowness of movement, patients may be prescribed Levodopa and dopamine agonists.
In addition, drugs that increase blood pressure will help support the improvement of orthostatic hypotension.

Usually, medications are of little help as multisystem atrophy progresses. Especially, for severe cases, most patients are not able to feed themselves and need the support of tube feeding.
5. Prognosis of multiple system atrophy
Statistically, the majority of patients with multisystem atrophy have a poor prognosis (with a median survival of 9 years from disease onset). Some of the poor prognostic factors can include:The disease begins when the patient is old. Patient is female. People with early autonomic failure. Shorter intervals between clinical milestones (eg, dysphagia, slurred speech, cognitive impairment, frequent falls, etc.) The disease is not directly life-threatening but causes many difficulties in the work and life of the patient. Therefore, patients as soon as they have symptoms need to see a doctor for diagnosis and timely intervention measures to prevent serious disease progression.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.