This is an automatically translated article.
The article was professionally consulted by Specialist Doctor I Nguyen Thi Man - Department of Obstetrics and Gynecology - Vinmec Danang International General Hospital. The doctor has more than 10 years of experience in diagnosing, consulting and treating in the field of Obstetrics and Gynecology.The CTG assessment is a systematic and comprehensive assessment. Any deviations beyond the normal curves should be recognized and analyzed in order to arrive at a correct conclusion during labor monitoring, to avoid late or inappropriate intervention. essential for mother and fetus. Therefore, fetal health monitoring by CTG plays an important role especially during labor.
What is CTG measurement? Measuring CTG is measuring fetal heart rate and uterine contractions with a fetal heart monitor called obstetric monitoring. The obstetrical monitor (or EFM) refers to the simultaneous recording of fetal heart rate and uterine contractions. The resulting plot is called a Cardiotocogram (CTG).
1. Normal and abnormal fetal heart curve
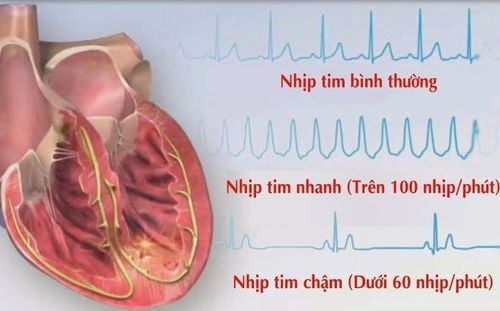
Cardiotocography (CTG) is performed during uterine contractions. On paper monitoring will record the progress of uterine contractions and fetal heart rate. So what is the normal fetal heart curve?If from 120-160 beats/minute for term pregnancy: Normal; If >160 beats/min: Tachycardia; Basal fetal heart rate between 100-120 beats/min: Suspicious; Basal fetal heart rate < 100 beats/min: Bradycardia. What is abnormal fetal heart curve? If it's over 160 beats, it's called tachycardia, or if it's less than 100 beats, it's called deceleration. In the range of 100-120, there are suspicious signs:
Bradycardia: the cause of the bradycardia is due to the mother taking drugs (lowering blood pressure), the mother has low blood pressure or shock, convulsions, hypothermia, premature rupture of membranes, premature rupture of membranes, umbilical cord compression, placental abruption, preterm pregnancy, fetal arrhythmia, complete atrioventricular block; Tachycardia: Tachycardia is often related to the fetus's ability to cope with some threat to health. Tachycardia without increased rhythms with decrease or loss of intrinsic oscillation, or late deceleration indicates severe fetal hypoxia; Causes of fetal tachycardia include: maternal fever, anxiety, hyperthyroidism, chorioamnionitis, fetal anemia, fetal viral infection or infection, fetal hypoxia, after a prolonged deceleration, after external anesthesia dura, cardiovascular pathology; Other typical baseline Fetal contours:
Shift of the Fetal baseline: Shift of the Fetal baseline can take place in an upward or downward direction. If ascending, it may be due to an infection in the uterus, the fetus is hypoxic from any cause (umbilical cord compression). Shift in the basal fetal heart rate during the 2nd stage of labor is often associated with low cord blood pH; Basal line undulation: Severe fetal bradycardia may be seen in cases of umbilical cord circulation obstruction, placental abruption, or maternal complications such as hypotension, shock, convulsions, uterine rupture, or myocele supply is overstimulated. In cases where the undulating baseline is present within a limited period of the normal fetal heart rate, it may also reflect fetal neurological damage; Baseline unknown: The baseline fetal heart rate could not be determined. The reason for the unknown baseline could be a series of increased beats, intrinsic hyperoscillation, successively variable decelerations, or fetal arrhythmia. Increased rate: Is an indicator of a healthy fetus, also known as a responsive fetal heart rate curve;
2. Some tests to assess fetal health by CTG
2.1 Non-Stress Test (NST) Is a chart recording the fetal heart rate in the absence of uterine contractions to investigate the response to subsequent increased fetal heart rate after fetal movements. The minimum execution time is 30 minutes. The test is done in the Fowler position, slightly left side. There should be a clear conclusion when reading the CTG; The presence or absence of a rising beat - satisfying the stated criteria for duration and amplitude - for a certain period of time from 20 to 30 minutes; Fetal heart rate is flat, internal fluctuations are lost. Estimating the percentage of the flat chart compared with the whole chart will help evaluate the prognosis of the fetus; If the stated conditions are strictly adhered to, the sensitivity of chromosomes reaches 97%; In contrast, in the face of an unresponsive chromosome, it is necessary to exclude fetal sleep (the average fetal sleep-wake cycle is about 70-90 minutes, of which the dormant phase lasts about 30 minutes), see Review the drugs being used, especially tranquilizers, as well as change the patient's position when doing chromosomes. An unresponsive chromosome has only an alarming value but not a diagnostic value. The positive predictive value of chromosomes is only 15%. Often will do more Stress test or strengthen the monitoring of fetal health.
If you have unusual symptoms, you should be examined and consulted with a specialist.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














