This is an automatically translated article.
Posted by Dr. Tran Hoang Ngoc Anh - General Surgery Department - Vinmec Central Park International General Hospital
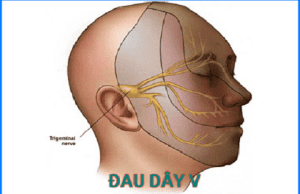
The term primary facial neuropathic pain has been described to include paroxysmal, episodic, unilateral facial pain and is localized to one or more branches of nerve V. The pathogenesis of this condition is controversial. argue
1. Make a problem
Primary neuralgia was first described by J.H.FEHR and J. LOCKE in the late seventeenth century. In 1756, ANDRE used the term “paroxysmal facial pain” to refer to primary neuropathic pain of the V nerve.
The term primary facial neuropathic pain was described to include pain in the face. intermittent, unilateral, and localized to one or more branches of nerve V. The pathophysiology of this pathology is controversial, but the typical clinical presentation helps to determine the diagnosis and uses laboratory tests to help determine the diagnosis. differentiate it from symptomatic facial neuropathic pain.
In recent years, with the development of medicine and especially the treatment regimen for nerve pain V resistant to medical treatment has been used in the past 15 years, including interventional techniques such as: Percutaneous interventional methods (thermocoagulation in the Gasser ganglion, injection of glycerol into the cerebrospinal fluid pool, insertion of the Gasser ganglion with a balloon), some authors use a direct approach such as (microsurgical partial resection of the branches). major nerves, microvascular decompression). However, each method presents advantages and disadvantages in implementation.
In the typical form, the diagnosis is relatively easy, clinical includes 4 factors:
2.1 Nature of pain
Intense and paroxysmal pain: Sudden onset of pain, most commonly an electric shock-like form , sometimes a crushed and torn form, but rarely a scalding form. This pain is usually short, lasting a few seconds, but can occur consecutively causing the pain to last for 1 to 2 minutes; The patient was completely normal between episodes. The frequency of the pain determines the severity of the disease.
2.2 Distribution of pain
The pain is unilateral, always localized according to the distribution of nerve V and is most commonly limited to one of the three branches. In 40% of cases, in the upper jaw, usually distributed below the orbit, the pain usually originates in the upper lip, in the nostrils or in the upper gums. In 20% of cases, the lesion is distributed to the mandible, usually confined to the chin nerve. Neuropathic pain is only distributed to the ophthalmic branch, distributed over the orbit (upper eyelid, base of the nose) in less than 10% of cases.
2. Clinical Manifestations and Diagnosis
2.3 Conditions of onset of pain
A fairly typical sign, but may not be present at times: Most often with direct nerve stimulation, mucosal areas rarely is called the “trigger zone”. The onset of attacks can also be indirect when talking, grimacing, laughing, or chewing. Each pain is separated by an aid of 1 or 2 minutes, which is the time when tactile stimuli are ineffective and the time that the patient can use to perform movements to avoid pain. onset of pain.
2.4 Other neurological signs are completely normal
As the fourth feature of the clinical presentation, it is absolutely necessary for the diagnosis. Primary neuropathic pain develops in an intermittent fashion: Episodes of pain are separated by periods of spontaneous remission that can last for several months or, in some cases, for several years. In fact, in some cases of nerve pain, the pain is followed by a facial pain that persists for several minutes, in the form of heat or burning, with transient redness of the face, watery eyes, and runny nose. . Progressive forms of primary neuropathic pain: In the course of neuropathic pain some of these features may be lost and may progress to a state of persistent severe pain. This clinical presentation may be emphasized in the patient's description, and the only factor in the inquiry, detection of exacerbations, is necessary for the diagnosis. There are also cases where a hypoesthesia is present. This case must be confirmed by multiple laboratory tests to confirm the diagnosis. Bilateral primary forms of neuropathic pain are very rare (5%) and are often secondary to the initial localization on one side. Each side proceeds differently, with attacks that don't work together. Usually, the diagnosis of primary neuropathic pain is easy, can only be made on inquiry, and errors are encountered due to erroneous approaches. The only difficulty encountered is defining the features of primary neuropathic pain. Diagnosis is difficult in symptomatic neuropathic pain when the clinical presentation is similar to the primary form. The distinction is made more difficult when there is a so-called "primary" form where anatomical factors are compressed, especially vascular, leading to an overlap between the primary pathology and the symptomatic disease. . Within this framework we must discuss what are called "atypical" cases of facial nerve pain, which may be associated with a typical paroxysmal pain that is sensitive to carbamazepine, or with a deep pain state. more or less episodic, or with an occasional combined and localized hypoesthesia according to the distribution of pain, or with both. In these cases, a complete bilan should be performed to look for the exact cause, the cerebellar pontine angle should be examined to look for a vascular entrapment of the nerve, and microvascular decompression should be performed. .
2.5 Subclinical diagnosis
The diagnosis of primary neuropathic pain is mainly clinical, not requiring a specific test in the typical case of V nerve pain.
2.6 Differential diagnosis
In the face of a case with atypical symptoms, we should look for the cause rather than diagnose primary V nerve pain as this could be a case of neuropathic pain V secondary (appears in all age groups, lesions are often tricuspid, persistent pain associated with exacerbations, often associated with decreased sensation and focal neurologic findings on examination).
Atypical facial neuropathic pain of trigeminal origin or other cases of facial pain not of V nerve origin including:
Cases of vascular pain of the face (often with onset of infancy In young children, pain is pulsatile, accompanied by sympathomimetic manifestations, lasting for many hours without regressing, lesions manifest mainly in the posterior orbit, occurring according to circadian rhythms and seasonality. Horton (with signs of local inflammation in the blood vessels) Cases of facial pain without neuropathic pain (sinusitis, glaucoma, iritis, toothache, facial tumors....) Pain Face due to psychological causes (presenting similar to a case of vascular pain of the face) In all cases, appropriate laboratory tests should be performed to look for the cause.

3. Pathogenesis
The pathogenesis of primary V neuralgia is controversial and controversial.
Currently, two hypotheses exist:
The “peripheral” hypothesis holds that primary V nerve pain arises from a lesion of the peripheral nerve, which is the basis for surgical treatment. The “central” hypothesis, under which this electric shock is essentially a paroxysmal discharge of the trigeminal nervous system, is compared to the electrical discharge in epilepsy (neuropathic pain). epileptic form of TROUSSEAU), who led the trial with antiepileptic drugs, used phenytoine first and then carbamazepine (BLOM, 1962). In practice, neither of the two hypotheses is convincing and it seems likely that central and peripheral factors combine to produce “primary” neuralgia.
Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit. and treatment of migraine, neuralgia at the Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
SEE MORE
Why do you have 5th nerve pain? Features of nerve pain V No. 8 nerve tumor: causes and treatment














