This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
As all professional associations recommend in guidelines, chronic HBV patients should receive antiretroviral prophylaxis when they are started on biologics that do not target TNF. In patients with resolved HBV, the rate of hepatitis B virus reactivation not receiving antiretroviral prophylaxis in patients receiving IL-23, IL-17, and JAK inhibitors turns up to 2.3%, 4.2% and 0%.
1. IL-23 . Inhibitors
Mechanism of HBV reactivation:
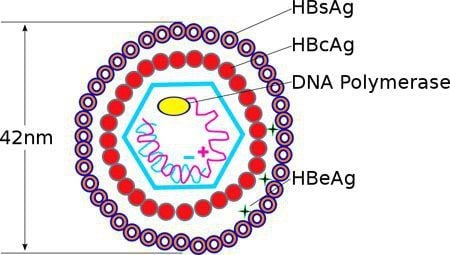
Specific IL-23 antagonists, such as tildrakizumab, risankizumab, guselku-mab, and brazikumab, have been shown to be effective against psoriasis and CD. These drugs bind to the p19 subunit on IL-23 and inhibit its interaction with IL-23 receptors. The underlying mechanism of hepatitis B virus reactivation in patients treated with IL-23 inhibitors remains unclear. Previous studies showed that 17 T cells, expanded by IL-23, increased with severity of liver injury in chronic HBV patients. An observational, clinical-controlled study also demonstrated that expression levels of IL-23 and IL-17 are associated with increased hepatitis B e-antigen (HBeAg) clearance and impaired HBsAg in HBeAg-positive chronic HBV patients during treatment with pegylated IFN. This study also shows that high serum IL-23 levels can predict response to IFN therapy in HBeAg-positive chronic HBV patients. Because TH17 cells promote B-cell differentiation and function, IL-23 may trigger humoral immune responses against circulating HBV and play a role in facilitating HBV clearance by IFN therapy. Although this hypothesis suggests that IL-23 inhibitors may decrease HBV clearance, it remains to be seen whether these drugs contribute to the development of hepatitis virus reactivation. B or not. Clinical studies in patients with autoimmune disease :
There are limited safety data on IL-23 inhibitors in patients with HBV infection. A case report found that a recovered HBV-infected patient did not develop hepatitis B virus reactivation 1 year after initiating guelkumab. No studies have been reported focusing on the risk of hepatitis B virus reactivation in patients treated with other IL-23 inhibitors.
2. IL-17 . Inhibitors
Mechanism of HBV reactivation:
IL-17 is a major TH17 cell-acting cytokine and mediates host defense mechanisms. Inhibition of IL-17 with secukinumab, ixekizumab, and brodalumab has demonstrated clinical benefit in patients with psoriasis, psoriatic arthritis, and ankylosing spondylitis. The TH17/IL-17 axis is involved in fibrinogenesis and increases the expression of proinflammatory cytokines, which promote the recruitment of inflammatory cells in chronic HBV patients. A previous study showed that Th17 cells were significantly increased in chronic HBV patients, as was the expression level of IL-17. They also demonstrated that inhibition of viral replication induced by IFN-α resulted in a decrease in TH17 cells and IL-17 expression, suggesting that TH17 cells may play an important role in this pathway. IFN-α treatment to eliminate HBV. As the authors described above, TH17 cells also facilitate B cells and will enhance the humoral response to clearly circulating HBV. These findings suggest that the TH17/IL-17 axis may be involved in HBV clearance and that its inhibition may increase the risk of hepatitis B virus reactivation. Clinical studies in patients with autoimmune disease:
A prospective multicenter study of 22 chronic HBV patients who did not receive antiretroviral prophylaxis after initiation of secukinumab revealed 6 diseases. patients (27.3%) develop hepatitis B virus reactivation. Three patients with hepatitis B virus reactivation started antiretroviral therapy and their viral load dropped rapidly within 3 months. The remaining three patients for hepatitis B virus reactivation were followed up without antiretroviral therapy and their viral load remained low without acute hepatitis. Notably, none of the 3 chronic HBV patients receiving antiretroviral prophylaxis developed hepatitis B virus reactivation. Therefore, this study reinforces the importance of Antiretroviral prophylaxis in chronic HBV patients initiating IL-17 inhibitor therapy. This study also included 24 patients with recovered HBV who did not receive antiretroviral prophylaxis and identified one patient (4.2%) who had a positive viral load at baseline. develop hepatitis B virus reactivation without acute hepatitis . This study reaffirms the EASL and APASL guidelines recommending antiretroviral prophylaxis in patients with recovered HBV if their baseline viral load is positive. A case report of a chronic HBV patient treated with ixekizumab and entecavir concomitantly did not develop hepatitis B virus reactivation after 18 months of treatment. Another report showed that a patient with recovered HBV did not experience hepatitis B virus reactivation during follow-up. Because data on the risk of hepatitis B virus reactivation in patients treated with ixekizumab or brodalumab are still limited, further studies with larger sample sizes are warranted.

3. JAK . Inhibitors
HBV reactivation mechanism:
JAKs bind to type I and II cytokine receptors and transmit extracellular cytokine signals to activate various signal transmitters and transcriptional activators, regulating controls the proinflammatory machinery of the cellular immune response. The clinical benefit of JAK inhibitors has been demonstrated in patients with rheumatoid arthritis, psoriatic arthritis, and ulcerative colitis. Important signaling pathways in host defense include innate antiviral responses mediated by IFN-α/β mediated by the JAK1-tyrosine kinase 2 complex and IFN-γ mediated JAK1-JAK2 complex. Thus, JAK inhibitors may counteract the inhibitory effect of IFN on viral replication. Furthermore, dendritic cells and efficient T cell lines including T cells and Tc cells play an important role in protecting against HBV infection. A previous study demonstrated that JAK inhibitors can suppress dendritic cell differentiation and function, leading to impaired T-cell activation. Therefore, it was suggested that inhibitors JAK may negatively interact with the defense mechanism against HBV infection. Further studies investigating how JAK inhibitors affect the development of hepatitis B virus reactivation are warranted.
Clinical studies in patients with autoimmune disease:
A retrospective cohort study including 6 chronic HBV patients found that 2 out of 4 patients (50%) were not receiving prophylaxis with Antiretroviral agents developed hepatitis B virus reactivation after starting tofacitinib. One patient had high ALT levels and was started on entecavir, resulting in decreased HBV-DNA and ALT levels. Another patient started entecavir and did not develop acute hepatitis. Both patients continued to take facitinib after developing hepatitis B virus reactivation. Meanwhile, 2 chronic HBV patients receiving antiretroviral prophylaxis did not develop hepatitis B virus reactivation after initiation of tofacitinib. Furthermore, in this study, none of the 75 patients with recovered HBV received antiretroviral prophylaxis and no hepatitis B virus reactivation was observed. in this group. Another study also demonstrated that patients with recovered HBV did not develop hepatitis B virus reactivation after initiating tofacitinib A study evaluating integrated data from four phase 3 trials of baricitinib in patients showed that, out of 215 patients with resolved HBV, 8 patients (3.7%) had a single quantitative outcome of HBV-DNA viral load (HBV-DNA level ≥29). IU/mL) after starting baricitinib. Of these 8 patients, 4 met the definition of hepatitis B virus reactivation (HBV-DNA ≥ 100 IU/mL), but none developed hepatitis. HBV-DNA at baseline was evaluated in 6 patients and all examined patients had no detectable HBV-DNA levels. Antiretroviral therapy was not used in 5 out of 8 patients All of these findings suggest that chronic HBV patients should receive antiretroviral prophylaxis when they are started on antiretroviral therapy. JAK mechanism. For patients with resolved HBV infection, since hepatitis B virus reactivation is sometimes reported even when their HBV-DNA levels are undetectable at baseline, further investigation is required. appropriate consultation with a hepatologist. There are limited data on the risk of hepatitis B virus reactivation in patients with autoimmune disease treated with other JAK inhibitors (eg, upadacitinib, filgotinib, peficitinib).
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.