This is an automatically translated article.
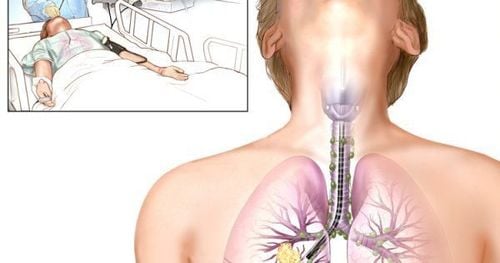
The article was professionally consulted with Master, Doctor Dang Xuan Cuong - Department of Emergency Resuscitation - Vinmec Hai Phong International General Hospital.Lung abscess is an acute necrotizing inflammatory condition that creates pus-filled foci in the lung parenchyma, which after embolism will form caverns in the lungs. To treat lung abscess effectively, it is necessary to choose appropriate antibiotics along with actively draining the lung abscess for the patient.
1. What is a lung abscess?
Lung abscess is an acute inflammation of the lung parenchyma not caused by tuberculosis, causing necrosis, destruction of alveolar membranes, capillaries, and formation of a pus-filled cavity.Patients with lung abscess often have reduced airway defense mechanisms. Normally, mucus in the nasopharynx containing bacteria can be sucked into the lungs during sleep, but a local lung defense mechanism will eliminate the bacteria. When this protective mechanism is reduced, lung abscess has conditions to develop. Decreased lung protection mechanism is common in immunocompromised people, alcohol abusers, tobacco users, exhaustion,...
2. Methods of diagnosing lung abscess
To diagnose a patient with a lung abscess, the doctor will rely on the following factors:2.1 Clinical symptoms of a lung abscess patient A lung abscess patient has the following clinical symptoms:
Fever 38.5oC , sometimes higher, may or may not be accompanied by chills. Chest pain on the affected side, patients with lower lobe lung abscess may present with abdominal pain. The patient coughs up purulent sputum. The sputum often has a stench, can spit a lot of pus, sometimes it can spit up pus and blood, and even cough a lot of blood. However, there are cases of only a dry cough. The patient has difficulty breathing, may show respiratory failure such as rapid breathing, purple in the lips, the tip of the extremities. On lung examination, crackles, moist rales, snoring rales can be seen, sometimes cavernous syndrome, condensate syndrome are seen. 2.2 Subclinical diagnosis The results of laboratory tests and diagnostic imaging of patients with abscessed pneumonia are as follows:
Blood count: white blood cell count increases, usually > 10 giga/liter, erythrocyte sedimentation rate increases. Chest X-ray: The chest x-ray image shows the abscess cavity usually has a relatively regular wall with air-fluid levels, can show 1 or more abscesses, unilateral or bilateral. It is necessary to take a lateral chest X-ray to determine the exact location of the abscess to help choose an appropriate method of drainage. Direct endoscopic staining and bacterial culture from sputum, bronchial fluid or abscess pus. Blood culture when fever >38.5oC, do antibiotics if bacteria are found. 2.3 Diagnosis of the cause The identification of the cause is based on the results of microbiological examination of sputum, bronchial fluid, blood or other specimens.
The causative agent of lung abscess is usually anaerobic bacteria, staphylococcus aureus, Klebsiella pneumonia, Pseudomonas aeruginosa, parasites (amoeba),... Favorable factors of the disease are immunocompromised patients due to HIV or due to the use of immunosuppressive drugs, alcoholism, tobacco addiction,...

Yếu tố thuận lợi của áp xe phổi là nghiện rượu
3. Treatment of lung abscess

Bệnh nhân áp xe phổi có thể được điều trị bằng kháng sinh
Types of antibiotics that can be used are:
Penicillin G used from 10-50 million units depending on the condition and weight of the patient, intravenous infusion 3-4 times a day. Use Penicillin in combination with an aminoglycoside antibiotic such as gentamycin (3-5mg/kg/day IM once) or amikacin (15mg/kg/day IM once or IV phase in 250ml NaCl 0.9 solution. %). Use Amoxicillin + clavuanic acid or ampicillin + sulbactam instead of penicillin G if beta-lactamase-producing bacteria are suspected, the dose is 3-6g/day. If lung abscess is suspected to be caused by anaerobic bacteria, one of the following combinations can be selected: beta lactam + clavuanic acid group 3-6g/day in combination with metronidazol dose 1-1.5g/day, intravenous infusion 2 -3 times/day or Penicillin G 10-50 million units combined with metronidazole 1-1.5g/day IV Penicillin G 10-50 million units combined with clindamycin 1.8g/day IV. If staphylococcal abscess is suspected, use Oxacillin 6-12g/day or vancomycin 1-2g/day. If drug-resistant staphylococci are suspected, combine the above drugs with amikacin. If Pseudomonas aeruginosa lung abscess is suspected: use Ceftazidim 3-6g/day in combination with quinolone antibiotics such as ciprofloxacin 1g/day, levofloxacin 750mg/day. If lung abscess is caused by amoeba, use Metronidazole 1.5g/day intravenously 3 times/day in combination with other antibiotics. 3.1.2 Draining the lung abscess The patient will be drained to make the amount of pus in the abscess drain out as much as possible. Methods of drainage of lung abscess include:
Postural drainage, thoracic pulsation: choose the most appropriate drainage position for the patient based on chest x-ray images or computed tomography scans. chest. Conduct postural drainage several times a day, at first, drain for a short time, then gradually lengthen depending on the patient's tolerance, the drainage time can be up to 15-20 minutes/time . Flexible bronchoscopy to aspirate pus in the bronchi to help drain the abscess. Puncture drainage of pus through the chest wall when the pulmonary abscess in the periphery does not communicate with the bronchi, the abscess is close to the chest wall or adheres to the pleura. A 7-14F catheter is inserted into the abscess to drain the pus through a continuous suction system. 3.2 Surgical treatment of lung abscess

ệnh nhân sẽ được phẫu thuật cắt phân thùy phổi hoặc thùy phổi hoặc cả một bên phổi tùy theo độ lan rộng với thể trạng bệnh nhân hoặc chức năng hô hấp trong giới hạn cho phép
Abscess >10cm Chronic treatment has no results. Patients with recurrent hemoptysis or severe, life-threatening hemoptysis. Abscess associated with severe focal bronchiectasis, with complications of bronchopleural fistula. During treatment, it is necessary to strengthen the diet so that the patient has enough health to fight the disease. To prevent disease, it is necessary to pay attention to oral hygiene, nose and throat. When there are infections of the teeth, mouth, nose and throat, they must be treated thoroughly. In particular, for patients who eat with a nasogastric tube, caregivers when feeding patients must closely monitor, to avoid the patient choking on food.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.