This is an automatically translated article.
The operating principle of PiCCO is based on the combination of transpulmonary thermodilution and continuous pulse contour analysis and measured PICCO parameters in blood monitoring. actions such as CO, preload, systemic resistance, cardiac contractility, and extravascular volume in the lungs without the need for a catheter in the right heart.1. Advantages of the PiCCO . method
Hemodynamic exploration by PiCCO method is a high-tech procedure applied in the resuscitation of patients with circulatory failure/acute circulatory failure, contributing to the diagnosis, treatment and monitoring of hemodynamic status. PiCCO is a new method with high applicability, fast, and few complications that can be applied in emergency departments.PiCCO (pulse contour cardiac output) is an advanced hemodynamic monitoring system. The operating principle is based on the combination of the transpulmonary thermodilution method and the continuous pulse contour analysis method, which measures continuously and simultaneously many hemodynamic parameters such as CO, pre-amplification. burden, systemic resistance, cardiac contractility, and extravascular volume in the lungs without the need for right-heart catheterization.
PiCCO uses a central venous catheter with a built-in heat sensor. The second part is a femoral artery catheter with an additional heat sensor. Cold water pumped into the internal jugular vein will follow the circulation from the central vein into the right atrium, down to the right ventricle. Then cold water will go up the lungs through the pulmonary artery into the urinary circulation, from there the cold water will return to the left atrium and left ventricle, the cold water will follow the thoracic aorta and down the abdominal aorta. There is a heat sensor at the abdominal aortic catheter that collects and reports to the microprocessor on the PiCCO. Since the blood temperature is always higher, thermal dilution occurs until the temperature returns to equilibrium.
PiCCO measures the following parameters:
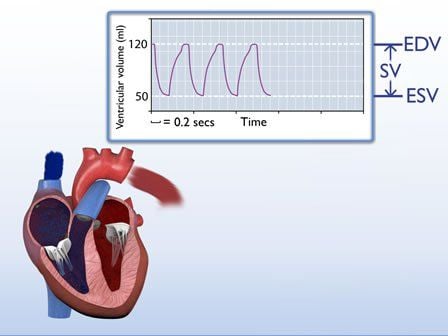
Continuous Cardiac Output Global End diastolic Volume (volume of blood in 4 chambers of heart) GEDV Intrathoracic Blood Volume (volume of blood in 4 chambers of heart + in pulmonary vasculature) ITBV Extravascular Lung Water EVLW Systemic Vascular Resistance SVR Stroke Volume Variation SVV
2. Designation

Chỉ định cho bệnh nhân có tình trạng huyết không ổn định: sốc, suy tim cấp
3. Contraindications
Contraindications for arterial and venous catheterization are: Contraindication of femoral artery with surgical interventions in the inguinal region (femoral artery transplant) or severe bilateral inguinal burns. Alternative arterial routes (axillary, brachial, radial) may be used.4. Clinical application

Ứng dụng lâm sàng của phương pháp PiCCO là đo cung lượng tim
4.2. Preload Many studies have confirmed that ITBV and GEDV have a higher accuracy than chamber filling pressure in assessing preload.
Cardiac filling pressures (Central Venous Pressure: CVP and Pulmonary Obstructive Pressure - PAOP) are commonly used to assess preload, but those parameters are imprecise. Because end-diastolic ventricular pressure is dependent on chamber relaxation, it does not faithfully reflect preload volume. On the other hand, CVP and PAOP were affected while the patient was on mechanical ventilation, while ITBV and GEDV were not significantly affected by artificial ventilation.
The transpulmonary heat dilution method has more advantages, no need for pulmonary artery catheter, compared with measuring left ventricular end-diastolic area by echocardiography, GEDV does not depend on the level of sonographer and can be carried out frequently and easily at the hospital bed.
4.3. Evaluating the response to fluids One of the most common challenges facing the resuscitator is the response of CO to an increase in circulating volume, which is so real that most studies only found that only 50% of patients in severe condition respond to fluids, and in a few others, infusions are harmful to the lungs and other organs. Because the correlation between preload and stroke volume depends on ventricular contractility. Isolated assessment of ventricular preload is not sufficient to predict response to perfusion.
Although increasing or decreasing variation of preload volume parameters is used in predicting fluid response, in cases where the measured values are within the normal range, they will not what to predict. Therefore, a variety of hemodynamic parameters have been applied to evaluate the effect of infusion on hemodynamics especially in mechanically ventilated patients with the effect of positive airway pressure on stroke volume. In patients with sedation, positive pressure ventilation during inspiration changes SVV and PPV. Similarly, since vascular pressure is proportional to left ventricular stroke volume, and the variability of pulse pressure due to ventilation is closely related to stroke volume, it is possible to predict cardiac response to perfusion.
PiCCO system automatically calculates PPV and SVV in each stroke by analyzing pulse waves. Based on PPV and SVV, it is possible to predict the response of CO to fluid infusion in heart surgery patients. However, it is important to keep in mind that PPV and SVV are affected by tidal volume, e.g. during mechanical ventilation with high tidal volumes (>15ml/kg) the measured tidal volumes are lower than they actually are. economic.
Monitoring fluid adjustment according to SVV and PPV is a good method to assess fluid response in patients using sedation and mechanical ventilation, suitable for patients under anesthesia during surgery, this is a big step forward. in patient follow-up.
4.4. Evaluation of myocardial contractility Accurate assessment of myocardial contractility at the bedside is not simple, as it depends on many factors, including preload and/or afterload. The ventricular ejection fraction is commonly used to assess the contractile function of the heart, which is the ratio of stroke volume to the left ventricular end-diastolic volume. Pulmonary thermal dilution measures GEDV, so the quotient between stroke volume and one-quarter of GEDV can estimate the total ejection fraction of the heart.
These parameters are calculated by the PiCCO method and can be used to assess whether the patient has impaired ventricular function or not. In addition, PiCCO can continuously assess left ventricular contractility by measuring dP/dtmax during the indicator injection phase.
Việc đánh giá chính xác sức co bóp của cơ tim tại giường là không đơn giản
The EVLW parameter is of great value in guiding fluid administration especially in patients with increased permeability of small pulmonary vessels (eg, infection). The PiCCO system measures EVLW along with CO, preload (GEDV) and fluid response (PPV and SVV) parameters that can guide fluid therapy and especially in difficult-to-assess situations. prices, helping to reduce mortality.
The current trend is to use the method of continuous cardiac output monitoring to be able to detect the earliest changes in cardiac output as well as other values, thereby providing early treatment. . In the PiCCO method, people monitor cardiac output and associated parameters as described above continuously, the technique of placement is relatively simple, less invasive, fewer complications, besides it It also provides parameters to monitor preload (GEDV), monitor the response to fluid replacement to increase cardiac output (SVV), monitor pulmonary interstitial fluid retention (EVLW). These parameters are quite new and also help more or less in resuscitation work in general and cardiovascular resuscitation in particular.
PICCO hemodynamic testing is currently being applied in many hospitals, including Vinmec hospital. Vinmec Hospital is equipped with the latest and most modern machines and a team of experienced doctors and nurses, so the success rate is up to 90%, complications are rare. From there, it is possible to provide an early treatment that is effective for the patient.
PICCO hemodynamic testing is currently being applied at many hospitals, including Vinmec Times City Hospital. With the most modern and new generation of equipment and machinery along with a team of experienced doctors and nurses, the success rate is up to 90%, complications are rare. From there, it is possible to provide an early treatment that is effective for the patient.
Customers can go directly to Vinmec Times City to visit or contact hotline 0243 9743 556 for support.