This is an automatically translated article.
Renal artery malformations include stenosis and occlusion of the renal artery, with an abnormal anastomosis between the artery and the vein, often congenital. The disease is common in the central nervous system.
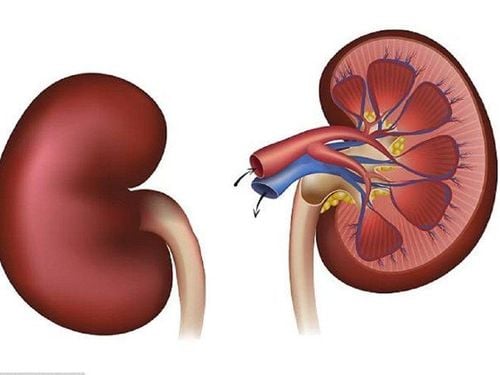
1. Renal Vascular Anatomy
Knowledge of renal vascular anatomy is important in understanding diagnostic studies and in planning treatment.
Renal artery is an organ branch that terminates from the aorta, branching into 4 or 5 renal arteries. The first branch is the posterior branch, which supplies the posterior segment of the kidney. The main artery then enters the renal tubule before dividing into other segmental branches.
These branches of the renal artery provide minimal collateral circulation between renal segments. The lobar renal arteries are located in the renal sinus and are branches of the segmental arteries.
The lobar arteries divide into the interlobular arteries, which are located in the renal parenchyma. The intersegmental arteries are located close to the collection system. The intervertebral arteries divide into the arcuate arteries and lead to the interspinous arteries.
Interstitial arteries lead to afferent arterioles to feed each glomerulus. Blood flows from the glomerulus to the outflow arteries, leading to the vascular rectum, thereby providing the renal venous drainage network.
Venous drainage follows an artery-like branching pattern. However, unlike the arterial system, significant connections exist between renal segments in the venous system.

Giải phẫu động mạch thận
2. What is renal artery malformation?
Renal artery malformations (AVMs), first described by Varela in 1928, are an abnormal communication between the venous system and the intrarenal arteries. They cause hematuria and are associated with hypertension. The disease is usually detected in young and middle-aged people (20-40 years old).
Renal AVMs can be congenital or acquired (usually iron-induced). Congenital renal AVMs are generally divided into the following 2 subtypes:
Cirsoid AVMs (more common): Usually larger than 1 cm in diameter and located adjacent to the collecting system. Cavernous AVMs are less than 1 cm in diameter and are usually located near the periphery. The aneurysm AVM is larger than 1 cm in diameter and located near the calyx. Cave AVM (less common). On the other hand, acquired renal artery anomalies are commonly referred to as renal artery fistulas (AVFs). Idiopathic renal AVFs have radiographic features of acquired fistulas, but no identifiable cause. They may be related to an intra-adrenal aneurysm that erodes the venous wall.
Renal AVMs are often identified during the evaluation of gross hematuria. Treatment can be tailored for each patient.
3. Pathophysiology of renal artery malformation
In cirsoid congenital AVMs, multiple communication between arteries and veins exists. These communications develop multiple coiled channels, forming a mass in the renal parenchyma. The communication vessels are tortuous, dilated and located below the cushion of the renal ureter. This vascular cluster forms a mass, with the arterial supply arising from one or more segmental or interbranch renal arteries.
The microscopic features of the arteries and veins involved resemble their normal soft tissue features. Occasionally, there may be some thrombosis involved. Their proximity to the collection system may explain the high prevalence of hematuria.
Less common congenital cavernous AVMs are characterized by arterial feeding into a cystic chamber, with a single venous drainage.
Acquired AVM is the result of traumatic disruption of the renal vessel. A tight connection between the arterial and venous systems occurs due to trauma.
Any renal AVM can lead to renin-mediated hypertension.
Dị dạng mạch máu não (AVM)
4. Causes of renal artery malformation
The etiology of congenital AVMs is unknown. In contrast, the etiology of acquired AVMs is generally known.
Percutaneous renal biopsy is the most common known cause of acquired renal AVF. An estimated 15-50% of biopsies result in some degree of fistula formation. In one study, where angiography was performed after each renal biopsy, radiographic evidence of fistula was identified in 15% of patients.
Trauma is another important, though uncommon, cause of acquired renal fistula. In hypertensive patients after renal injury, renal AVMs may occur in up to one-third of patients. In patients with penetrating trauma, AVFs may affect up to 80% of patients with post-traumatic hypertension. Trauma during ureteroscopy, percutaneous nephrolithectomy, or after partial nephrectomy has been described as the cause of intra-adrenal AVF.
Idiopathic AVF is thought to arise from spontaneous erosion or rupture of the renal artery into a nearby renal vein.
AVM can also occur in the setting of malignancy. Renal cell carcinoma with vascular deviation, with renal varices and parasitic tumor vessels both relatively common. Tumor-inducing factors are implicated and may explain the development of AVMs in renal tumours.
5. Epidemiology of renal artery malformation
Renal AVM is uncommon. The estimated incidence in large autopsy series is less than 1 case per 30,000 patients. In clinical studies, which often include patients evaluated by urological or vascular imaging techniques, incidence ranges from 1 case per 1000 patients to 1 in 2500. They account for less. 1% of all AVMs in the general population.
Congenital AVMs account for less than one-third of renal AVMs. Most of these are classical cirsoids. Congenital cirsoid AVMs have a dilated, spiral shape, resembling a dilated vein. Cavernous AVMs, with dilated vessels, account for the remainder of the congenital malformations.
Acquired AVF is the most common and represents 75-80% of renal AVMs.
Idiopathic renal AVF accounts for less than 3% of renal AVMs.
The international prevalence of renal AVMs is influenced by the prevalence of percutaneous renal surgery and biopsy because these interventions cause most of the acquired renal fistulas.
6. Clinical renal artery malformation
Gross hematuria is the initial sign or symptom in most (75%) patients with renal artery malformation (AVM). Renal colic may be the result of obstructing blood clots, which can be pronounced as mottled (worm-like) masses. Rarely, during the evaluation of asymptomatic microscopic hematuria, AVM is found and assumed to be the cause of hematuria. A significant proportion of patients with renal AVMs have hypertension. Half of patients with acquired AVM and one-quarter of patients with congenital renal AVM have high blood pressure. Prostatic hypertension is believed to be a risk factor for developing fistula after renal biopsy. Conversely, the hypertension that develops after biopsy may be due to increased renin secretion caused by hypoperfusion relatively distal to the AVM. Cardiac enlargement, congestive heart failure (CHF), or both may also be present in patients evaluated for renal AVMs. Rarely, a patient may experience hypotension due to bleeding from the AVM. This has been described in many contexts, including during pregnancy. Occasionally, renal AVMs can mimic renal cell carcinoma and can only be identified on surgical pathology. In rare cases, back pain is associated with the AVM.
AVMs have also been found to impair kidney function in patients with chronic kidney disease.
History of previous kidney biopsy or percutaneous renal surgery is an important risk factor for the development of acquired arteriovenous fistula (AVF). A history of kidney injury, especially penetrating trauma, is also an important risk factor for developing renal AVF.
Physical assessment may demonstrate findings of a flank injury. A palpable mass is often present in patients whose renal tumor is the cause of the fistula.

Tình trạng đái máu tổng thể có thể là triệu chứng của bệnh nhân bị dị dạng động mạch thận
7. Treatment of renal artery malformation
The initial approach to treating renal artery malformation (AVM) is usually guided arterial embolization. One indication for the treatment of these malformations is pain. Pain from renal AVM is due to systemic obstruction by a blood clot or to dilation of renal cysts due to intrarenal hemorrhage. Persistent gross hematuria, especially in anemic patients, can be treated promptly.
Hypertension is an important indication for treatment. Attempts were made during surgery before determining whether malformation was the cause of the hypertension. However, selective renal vein renin levels have not been successful in helping to determine which hypertensive patients will respond to embolization or nephrectomy.
Congestive heart failure (CHF) is an unusual but compelling indication. Several case reports have described patients with severe heart failure whose heart health improved to within normal limits after nephrectomy or AVM embolization.
Indications for surgical treatment have become more limited as the ability to treat renal AVM by embolization has improved. AVMs due to malignancy often require surgical resection. Significant metastatic disease and poor performance status may limit the use of nephrectomy, in which embolization can be palliative. Symptomatic hematuria that is difficult to embolize is definitively treated with nephrectomy. In most cases, hypertension is cured by nephrectomy. Ultimately, pain that is not resistant to less invasive efforts may respond to nephrectomy.
There are very few contraindications to the treatment of renal AVMs. Contrast allergy may require pre-treatment with antihistamines and non-steroidal anti-inflammatory drugs. Otherwise, renal AVM embolization is well tolerated, even in patients who cannot tolerate surgical intervention. However, in patients with poor general health, especially in cardiopulmonary status, surgical intervention may be contraindicated.
In addition, renal function must be carefully assessed before performing nephrectomy in selected patients. The importance of nephronectomy is enhanced in patients with underlying renal failure. Approximately 20-25% of renal units should be saved if possible. This provides an estimated glomerular filtration rate (GFR) of 10-15%, which may preclude many patients from needing dialysis for end-stage renal disease (ESRD). However, ultrafiltration damage can occur when less than 25% of the total renal mass is excreted.
Therefore, in patients with isolated kidney, bilateral AVM, or renal failure, detailed planning is necessary. These patients have an increased risk of partial nephrectomy. In addition, a strong argument can be made for routine use of nephron-sparing approaches, particularly for benign diseases such as renal AVM, in all patients when technically feasible. This helps to protect the patient from the small risk of developing kidney failure in the future.

Trường hợp bệnh nhân bị dị ứng thuốc cản quang có thể được điều trị thuốc kháng histamin
Non-surgical treatment In some cases, conservative therapy can be used safely. If resection is not performed at the time of angiography, observation is indicated in some patients. If symptoms and hemodynamic complications do not develop, noninvasive therapy is worth trying in patients with small AVMs. Hematuria usually improves with bed rest. Painkillers may be needed.
Little is known about the natural history of untreated AVMs. Acquired arterial fistulas (AVFs) tend to resolve on their own. One report described the spontaneous resolution of AVMs. The angiographic findings helped confirm radiographic disappearance of the malformation without specific intervention. However, theoretical concerns are that the therapy is expected to carry the risk of slowing bleeding due to an enlarged AVM or the development of irreversible hypertension. Because patients with AVM often present with symptoms, most patients are managed with definitive treatment rather than observation alone.
Medical management is essential to optimize outcomes. In addition to pain relief, hypertension should be treated. Heart failure must be controlled prior to surgical intervention. Blood transfusions may be required in rare patients with AVM bleeding. Finally, renal failure may occur as a complication of the contrast agent used during radiographic evaluation.
Initial therapy for AVMs is usually malformation-guided embolization. Many substances were injected in the attempt to remove the AVM. Initial attempts to embolize were complicated by recurrent AVMs. This is thought to be due to the type of material used to embolize the vessel. Materials that have been used for embolization include steel coils, autologous blood clots, gelatin sponges and foams, and synthetic polymers.
The most effective material for embolization seems to be absolute alcohol, which is relatively inexpensive. It is also easier to inject through the catheter lumen than many synthetic materials. Balloon catheters are used to occlude the feeding artery to prevent retrograde movement of the alcohol. Alcohol denatures the proteins in the wall of the AVM, thereby causing thrombosis and occlusion of malformations. In addition, the use of absolute alcohol for embolization has a hypotensive effect because it destroys the glomerular apparatus, eliminating the overproduction of renin that causes hypertension.
Surgical therapy The most likely treatment for AVM is removal of the entire kidney. Total nephrectomy is indicated for large cirsoid AVMs. In most cases, nephrectomy is reserved for patients for whom more conservative therapy has failed. If the fistula is due to malignancy, radical nephrectomy is usually indicated.
The main criticism of nephrectomy for renal AVMs is that a significant amount of normal kidney tissue is removed. Therefore, regenerative approaches have been advocated in selected cases. Partial nephrectomy has been accepted as a safe treatment for microscopic lesions. With increasing experience with partial nephrectomy for malignancy, partial nephrectomy will likely be performed with greater confidence, even for large and centrally located AVMs. In addition, to reduce morbidity due to the incisions required for renal surgery, laparoscopic partial and total nephrectomy have been used with increasing frequency to treat selected renal AVMs. .
In addition to partial nephrectomy, other techniques have been used to treat renal AVMs. Small malformations located in the periphery of the kidney can be treated by ligation of the feeding vessels. Dissecting the feeding vessels can be technically difficult. Bench surgery with auto-implantation can facilitate the successful treatment of large or central malformations. This degree of renal remodeling is rarely needed but can preserve enough renal tissue function to avoid dialysis in certain circumstances.
Although the most successful treatment for renal AVM, surgical intervention is usually reserved for difficult-to-embolize cases or those associated with malignancy.

Phương pháp phẫu thuật nội soi cắt một phần và toàn bộ thận điều trị các AVM thận đang rất được lựa chọn hiện nay
8. Possible complications
8.1 Complications of surgery Potential complications of nephrectomy can be classified by organ system, as follows:Heart - Arrhythmia due to electrolyte imbalance due to diuresis, ischemia due to surgical ischemia or anesthetic-induced hypotension; Lungs - Atelectasis, pneumonia, pneumothorax, pulmonary embolism; Gastrointestinal (GI) - Intestinal obstruction, pancreatitis, duodenal injury (due to contracture strain); Neurologic - Injury to the nerve below the ribs, stroke; Infectious (uncommon) - Foley catheter cystitis, surgical site infection, pneumonia; Partial nephrectomy has more potential complications. Bleeding after partial nephrectomy is more common than after total nephrectomy. Postoperative US Doppler may be useful to prevent hemorrhagic complications after partial nephrectomy; Renal failure has also been reported to be more common after partial nephrectomy. This occurs most often in pre-existing kidney failure, which may require partial nephrectomy; Acute tubular necrosis may occur; Cooling the kidneys during partial nephrectomy may reduce the duration and severity of acute tubular necrosis after partial nephrectomy. However, the necessity of renal cooling during partial nephrectomy is increasingly controversial. In experienced centers, laparoscopic partial nephrectomy can be performed without cooling the renal surface and without significantly increasing the risk of acute tubular necrosis. However, the application of laparoscopic partial nephrectomy in the treatment of renal AVM has not been clearly described. 8.2 Complications of Embolism Complications after embolization include pharmacological and technical factors. Contrast-induced nephropathy and serious allergic reactions can occur. Furthermore, the agent used for embolization can cause complications. The agent may migrate or be misdirected and thereby damage normal kidney tissue or other organs. A case description documented erosion of the coil and guide wires into the colon. Alcohol can cause transient headaches and mild intoxication.
May recur or leak continuously. Hematoma and pseudoaneurysm at the site of puncture (usually the femoral artery) are not uncommon, with clinical evidence of hematoma occurring in approximately 5% of patients.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.