This is an automatically translated article.
Shock is a state of circulatory collapse due to various causes, reducing or stopping the supply of blood and oxygen to the organs, especially vital organs such as the heart, lungs, and brain. This is a dangerous condition that requires medical staff to have a timely and positive handling attitude to be able to save the patient's life.1. Overview
The most common obstetric shock is hemorrhagic shock in obstetrics (postpartum haemorrhage, hemorrhagic miscarriage, ruptured ectopic pregnancy...) or due to infection (postpartum infection, septic abortion... ).Common type of shock in obstetrics
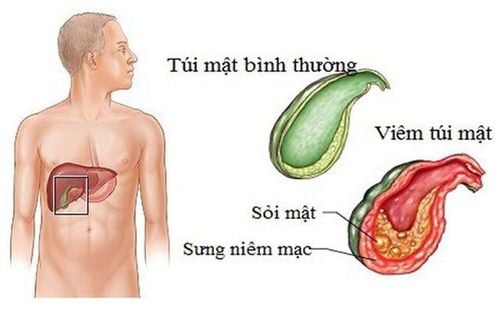
1.1 Shock due to blood loss Ectopic pregnancy Uterine rupture Genitourinary tract and perineal tearing Placental defect Uterine stagnation Placenta placenta Placenta abruption 1.2 Septic shock In obstetrics and gynecology, shock Infections are often caused by:
Common in unsafe abortions. Postpartum vegetables. Pre-existing infection in the fallopian tubes and fallopian tubes, or the genital tract. Late uterine rupture. 1.3 Shock due to amniotic fluid embolism Embolism due to amniotic fluid is uncommon, can be encountered in normal delivery or requires surgical intervention with fork-ripple, or cesarean section. Clinically, there are often three prominent syndromes: dyspnea, cardiovascular collapse, coagulation disorders.

Biểu hiện lâm sàng của bà bầu sốc sản khoa là vã mồ hôi, nhịp thở nhanh nóng,..
Drop in blood pressure < 90/60 mmHg. Pale skin (around the lips, eyelids, and palms). Sweating. Cold hands and feet due to peripheral vasoconstriction. Rapid shallow breathing (respiratory rate is usually more than 30 breaths/minute). Drowsiness, restlessness, or coma. Oliguria or anuria. Depending on the cause of shock, there are different clinical manifestations. Initial management Before a case of shock, initial aggressive management is very important to save the patient from the crisis.
Calling people to help and give first aid to the sick. Check vital signs: pulse, breathing rate, temperature. Make sure the airway is clear by placing the patient in a supine position (or turning to one side if the patient is vomiting). Aspirate sputum if the patient produces a lot of sputum and give the patient oxygen through the nose at a rate of 6-8 liters / min. At the commune level, if there is no oxygen tank, it is possible for the patient to breathe oxygen through an oxygen bag, it is best to give oxygen through a water tank to ensure enough humidity. To compensate for volume by rapid intravenous infusion of isotonic solution (Ringer lactate), sugar solutions should not be used to restore volume. In case of emergency, it is necessary to set up multiple transmission lines at the same time. The rate of infusion can be up to 1 liter of fluid in 15-20 minutes, 2 liters of fluid must be infused in the first hour. Try to rehydrate at a rapid rate in the case of hemorrhagic shock, the volume of fluid needed to be replaced is 2-3 times the volume of blood lost. In case of haemorrhage, it is necessary to stop the bleeding immediately and consider a blood transfusion for the patient. The decision of blood transfusion or not is mainly based on clinical and hemoglobin test <50g/liter. Check vital signs every 15 minutes. Check blood count, liver and kidney function, coagulation factors... In case of septic shock, blood culture, fluid culture to find the cause of the disease, then immediately use broad-spectrum antibiotics and combination of antibiotics antibiotics, when the antibiogram is available, use the drug according to the antibiogram. Treatment according to the cause of shock After the patient has stabilized with initial treatment, the cause of shock should be determined.
Shock from blood loss Determine cause of bleeding and treat bleeding immediately: Bleeding can be caused by miscarriage, ectopic pregnancy or ruptured ectopic pregnancy. Bleeding may also occur in the last months of pregnancy or in labor such as placenta previa, placental abruption, uterine rupture, postpartum genital tract trauma, or uterine atony, causing haemorrhage. In these cases, it must be quickly either with medication or with a procedure or surgery to stop the bleeding. Transfusion of blood as soon as possible compensates for the lost circulating volume. Cardiovascular support: Intravenous Dopamine Anticoagulation disorders by using antifibrinolytic drugs and blood products. Septic shock and toxicity Intramuscular high-dose combination antibiotics (possibly ampicillin 1g and gentamycin 160 mg), initial intensive care and referral. Oxygen, intravenous fluids. Heart aid. High-dose antibiotics in combination and according to the antibiogram. Treat the cause of infection: Drain the pus, remove the infection (hysterectomy).
2. Prevention

Không nên để sản phụ làm việc đến tận ngày đẻ

Không nên thăm khám thai qua âm đạo quá nhiều khi không cần thiết
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.