This is an automatically translated article.
An anticholinergic is a medicine that blocks the bad action of a neurotransmitter called acetylcholine. Before using anticholinergic drugs, patients need to know how to use them safely and effectively.
1. What is Cholinergic?
Cholinergic is known to contain chemical compounds capable of mimicking the function of acetylcholine. These agents are also capable of mimicking the function of butyrylcholine. So what is choline? "Choline" is understood as a component of the neurotransmitter acetylcholine. The parasympathetic nervous system is said to be purely cholinergic because it uses acetylcholine almost exclusively to send messages between cells and targets. In addition, neuromuscular and gestational neurons have cholinergic junctions of the sympathetic nervous system. Cholinergics are also receptors of merocrine sweat glands.
A substance or ligand that can induce or alter the release of acetylcholine or butyrylcholine is also called a cholinergic agent. In addition, if a receptor or a synapse uses acetylcholine as a neurotransmitter, they are also named a cholinergic agent.
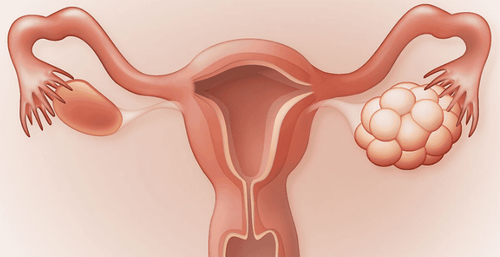
2. What is cholinergic urticaria?
Cholinergic urticaria is also known as choline urticaria. This is a type of physical urticaria, caused by the action or stimulation of physical factors. Triggers in cholinergic urticaria are heat and perspiration. Although this disease is not life-threatening, it affects the patient's quality of life.3. When are anticholinergics used?
Anticholinergic drugs are used in the following cases of treatment:
- Treatment of chronic obstructive pulmonary disease - COPD;
- Treatment of overactive bladder and incontinence;
- Treatment of digestive disorders;
- Treating the symptoms caused by Parkinson's disease,...
For each type of disease, the doctor will determine the appropriate anticholinergic drug for each patient and prescribe the dose and duration of drug use to the most effective treatment.
Anticholinergics come in many different classes of drugs. Some drugs with anticholinergic properties are antiemetics (Promethazine), Parkinson's drugs (Benztropine), gastrointestinal antispasmodics (Propantheline), bladder antispasmodics (Oxybutynin, Tolterodine), and antispasmodics. depression (Imipramine)...
4. Side effects of anticholinergic drugs
The treating doctor will prescribe an appropriate and safe anticholinergic drug, however, some patients may still experience side effects of the drug during use. Possible side effects depend on the individual's medical history, dose and dose, and the type of drug containing the anticholinergic.
Symptoms that are side effects of anticholinergics can be confusion, hallucinations, drowsiness, sedation, dry mouth due to decreased salivation, blurred vision, difficulty defecating, little secretions sweating more than usual and body temperature rising (causing heatstroke), memory loss,...
If the patient takes anticholinergic drugs with alcohol or more than the prescribed dose can cause conditions such as dizziness, feeling drowsy all the time, fever, severe hallucinations, difficulty breathing, rapid heart rate can even lead to death. If patients experience one of these conditions, they should stop using the drug immediately and notify the treating doctor or immediately go to the nearest medical facility for timely medical support.
Because of the possible side effects and even the risk of death, patients should not self-administer anticholinergic drugs but need to consult a doctor. Before prescribing for a patient to use, the doctor also needs to carefully consider the age, medical condition and drugs the patient is taking to prescribe the most appropriate.
5. Use caution with the elderly
Due to the large depletion of Cholinergic neurons or receptors in the brain, the central nervous system of the elderly is very sensitive to the side effects of drugs, especially to anticholinergic drugs. . Besides, the ability to break down and excrete drugs by the liver and kidneys in this group of people is also reduced, thus increasing the permeability to the brain through the blood. These are the main causes of anticholinergic side effects in this group of people.
Studies show that long-term use of anticholinergic drugs in the elderly group will increase the likelihood of dementia, impaired cognition, especially for anticholinergic antidepressants, antipsychotics, antiparkinsonian drugs, and antiepileptic drugs. These drugs can cause confusion, and the risk increases with the large number of anticholinergics the patient takes.
To avoid the risk of cognitive decline in the elderly, prescribing treatment should start with a low dose and then assess the possibility of treatment response to determine the most effective dose. In addition, patients should also be periodically tested for cognitive ability for any therapeutic purpose, including non-neurological conditions.
For the elderly population, alternative drugs without anticholinergic properties can be used to reduce the risk. During treatment, the patient should not be allowed to stop taking the drug suddenly, because this may cause more harm. Concerns about medication should be discussed with the doctor to be explained and better understand the benefits or risks of the treatment that the patient receives.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.