This is an automatically translated article.
Laparoscopic pancreatectomy and endoscopic tail resection are often performed in cases where the cancer in the pancreatic body and tail is still localized and has not invaded surrounding blood vessels and vital organs. Laparoscopic surgery is less invasive, helping patients less pain and faster recovery.
1. When is laparoscopic surgery to remove the body and tail of the pancreas?
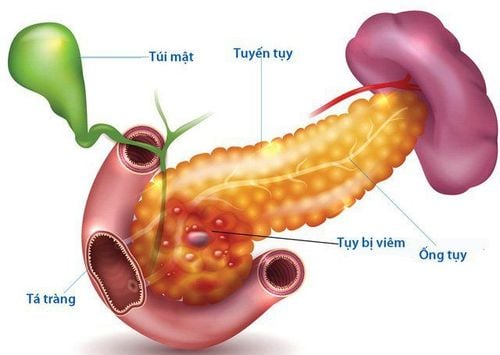
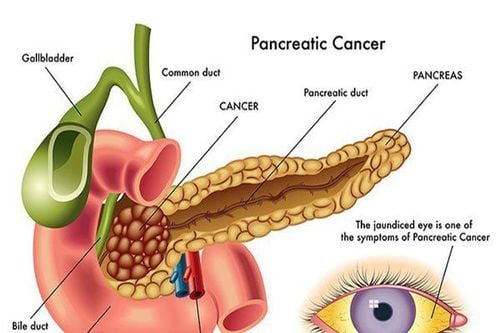
The pancreas is located in the upper abdomen, across the front of the spine and behind the lower part of the stomach. The pancreas is a long and slender organ, divided into 3 parts in order from left to right: the head of the pancreas, the body of the pancreas, and the tail of the pancreas. Pancreas has two extremely important functions, exocrine function and endocrine function. In terms of exocrine function, the pancreas produces digestive enzymes involved in the digestion of food. In terms of endocrine function, the pancreas produces and secretes into the bloodstream the hormones insulin and glucagon that help control blood sugar.
Laparoscopic body and tail resection is surgery performed laparoscopically to remove the entire body of the pancreas and to remove the tail of the pancreas excluding splenectomy. Depending on the individual case, surgery may or may not include radical lymph node dissection.
Laparoscopic pancreatectomy and laparoscopic tail resection are indicated in cases when:
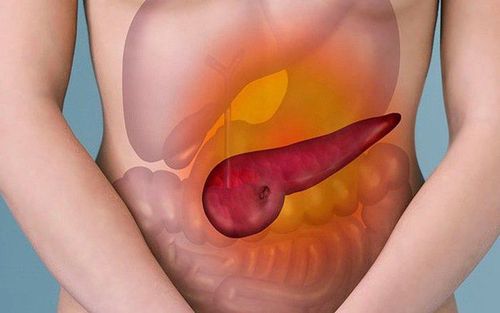
Cancer of the body or tail of the pancreas Benign tumor of the body or tail of the pancreas is at risk of malignancy True cyst of the body or tail of the pancreas Traumatic rupture of pancreatic body or tail Surgery is contraindicated in cases where pancreatic cancer has invaded important vascular structures such as the hepatic artery, superior mesenteric vascular bundle, or has metastasized to the peritoneum. In addition, patients with peritonitis due to late rupture of the body or tail of the pancreas, patients with active acute pancreatitis, or those with respiratory or cardiovascular diseases with contraindications to intra-abdominal inflation also This surgery should not be performed.

Bệnh nhân ung thư thân hoặc đuôi tụy cần được phẫu thuật
2. The process of laparoscopic surgery to remove the body and tail of the pancreas
2.1. Preparation for laparoscopic pancreatectomy and laparoscopic tail removal
Before laparoscopic pancreatectomy and laparoscopic tailectomy, the patient will have a clinical examination, perform a number of preoperative tests to ensure that the patient is healthy enough to participate in the surgery. Imaging techniques such as CT scan of the abdomen with injection, MRI of the abdomen with magnetic contrast or endoscopic ultrasound are indicated to assess the extent of pancreatic damage or to assess the stage of cancer. . Tumor biopsy guided by ultrasound or CT scan is indicated in some cases to confirm the preoperative diagnosis. Patients should use oral colonic lavage to clean the colon before surgery if there are no contraindications.
The medical staff will explain to the patient and family the purpose of the surgery, the possible risks. In order for the surgery to take place, the patient or his/her representative must sign a written consent to the surgery.
2.2. Steps to perform laparoscopic pancreatectomy and endoscopic pancreatectomy
The patient lies supine on the operating table, legs apart and knees bent. The surgical team performed endotracheal anesthesia, urinary catheter and nasogastric tube. The main surgeon stands on the right, the laparoscopic machine is placed on the left towards the patient's head.
The surgeon places 5 trocars, in which:
1 trocar 10mm placed at the navel with a scope 1 trocar 5mm placed in the right hip anterior axillary line 1 trocar 12mm placed at the level of the navel right midclavicular line 1 trocar 5mm placed on the hip left anterior axillary line 1 trocar 5mm placed at the level of the navel at the left midclavicular line Through the image on the screen obtained from the camera, the doctor will examine the abdomen to assess the stage of the cancer such as size, condition invasion, liver metastases, peritoneal metastases,... Move the patient to the right-angled high-head position, hanging the liver to have a favorable surgical field.
Depending on each case, the surgeon will choose one of two methods to cut the body and tail of the pancreas: cutting according to the anatomy at the boundary between the head and the body of the pancreas; and non-anatomical resection, which is the surgical removal of the pancreas, leaving part of the body of the pancreas.

Trước khi phẫu thuật cắt thân tụy nội soi và cắt đuôi tụy nội soi, người bệnh sẽ được khám lâm sàng
2.2.1. Laparoscopic pancreatic body and tail endoscopic resection according to anatomy
The primary surgeon cuts the gastrocolic ligament into the omentum omentum to expose the entire pancreas. To expose the superior mesenteric vein, the surgeon will perform a dissection along the bundle of the vessels of the middle colon to the lower border of the pancreas. Dissect immediately the pancreatic neck behind the pancreas and in front of the superior mesenteric vein up to the superior border of the pancreas. The auxiliary surgeon lifts the stomach and pulls the pancreas downward, and the primary surgeon dissects and removes lymph nodes (if cancerous) along the hepatic artery and branches of the visceral artery at the superior border of the pancreas. Next, the portal vein was exposed on the lateral border of the pancreas, tunneling posteriorly to the neck of the pancreas and anteriorly to the superior mesenteric and portal veins. Thread the wire to raise the pancreatic neck separate from the superior mesenteric and portal veins. Using a straight splicing machine, cut across the neck of the pancreas. Dissection of the body and tail of the pancreas from left to right, from bottom to top. Resection of the entire body and tail of the pancreas, preserving the spleen and splenic vascular bundle. Check hemostasis, enhance pancreatectomy, and dissolve monofilament. Put the specimen in the bag. Drainage by the apex of pancreatectomy.
2.2.2. Non-anatomical laparoscopic pancreatectomy and laparoscopic tail resection
The doctor cut the gastrocolic ligament into the omentum omentum to expose the entire pancreas. Perform dissection from left to right and from bottom to top, ligation of the dorsal branches of the pancreas along the splenic vessel bundle, lowering the transverse mesentery from the lower border of the pancreas. Continue dissecting to the position of the pancreatic body to be removed, using a straight splicing machine to cut across the body of the pancreas.
Check hemostasis, strengthen the apex to cut the body of the pancreas, put the patient in the bag.
Drain the splenic fossa or the edge of the pancreatectomy. Surgery left part of the body of the pancreas. The umbilical trocar incision is enlarged or opened with a small opening in the abdomen to remove the specimen.

Phẫu thuật cắt thân tụy nội soi và cắt đuôi tụy nội soi
3. Follow-up and care after laparoscopic pancreatectomy and endoscopic pancreatectomy
After surgery, the patient will be given pain relievers and antibiotics to prevent infection. Postoperative intravenous nutrition ensures adequate daily energy supply, adequate protein, albumin, blood transfusion, and adequate hydration and electrolyte replacement. On the first day after surgery, the patient can drink sugar water and milk. Patients will be able to eat soon after having a bowel movement.
4. Handling common complications during and after laparoscopic surgery to remove the body and tail of the pancreas
Common complications in surgery are uncontrolled bleeding or large tumors that cannot be operated by laparoscopic surgery, these cases are often converted to open surgery for treatment. Another fairly common complication is damage to the transverse colon when resection of the gastrocolic ligament. Depending on the extent of the injury, the doctor may stitch up the perforation through the endoscope or open the colon to the skin to stitch the wound.
Common complications after surgery are:
Abdominal bleeding: If bleeding is severe, the patient will be re-operated immediately by laparoscopic or open surgery. Pancreatic fistula: Treat conservatively in most cases. If the pancreatic fistula creates an intra-abdominal abscess or peritonitis, the patient is indicated for surgery. Postoperative intestinal obstruction: If it occurs, the patient will be treated as mechanical intestinal obstruction.
MORE
Chronic pancreatitis: How is it treated? How dangerous is acute pancreatitis? Acute pancreatitis progresses rapidly, the risk of death is high