This is an automatically translated article.
Laparoscopic rectal balloon lowering and anal reconstruction is a technique that can be indicated for all anorectal malformations in children, except for anorectal fistula or vestibular fistula.
1. Surgical treatment of anorectal malformations in children
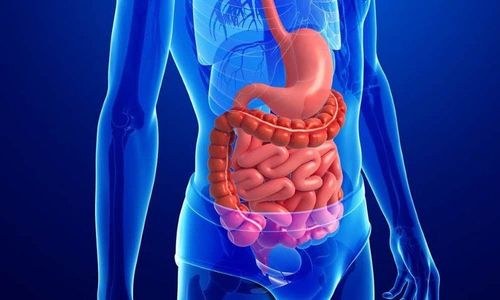
Anorectal malformations are one of the most common congenital malformations of the gastrointestinal tract, occurring with an incidence of 1/5000-1/4000 births. The incidence of anorectal malformations is similar between boys and girls.
When the fetus is less than 8 weeks, the rectum and bladder are still connected in a cavity called the slime cavity, the bottom is sealed with a slime membrane. Then, in the process of forming organs, the slime membrane is dissolved to form the gastrointestinal-genital-urinary tract organs connected to the outside, the urinary-rectum septum forms and develops downwards. divides rectum into urogenital mass. If there is an abnormality in the division, it will cause an anorectal malformation.
Signs of newborns with anorectal malformations are manifestations of postpartum bowel obstruction syndrome such as distended abdomen, vomiting, not passing meconium, a few still passing meconium. fistula, anal stenosis. Children with anorectal malformations, if not treated promptly, will lead to many dangerous consequences such as intestinal obstruction, intestinal rupture, secondary colonic dilatation, regurgitation into the respiratory tract causing respiratory infections, cause sudden death,...
Most anorectal malformations are treated with surgery. Depending on the degree of anal stenosis of each child, the doctor will choose the appropriate surgical method.
Laparoscopic rectal balloon lowering and anal reconstruction is a technique that can be indicated for all anorectal malformations, except for anorectal fistula malformations or vestibular fistulae. Currently, this surgery is often performed for cases of rectal bladder fistula and rectal prostatic fistula.
There are some contraindications to this surgery, which are children with bronchitis, pneumonia, blood clotting disorders or children with respiratory and cardiovascular diseases that are contraindicated with inflatables. Abdominal.

Trẻ em bị viêm phế quản chống chỉ định phẫu thuật nội soi
2. Laparoscopic surgery to lower the ball of the rectum and shape the anus
2.1. Preparing for surgery
Before surgery, the child will have a full body examination to detect coordination abnormalities, including:
Examination of the pelvis and sacrum to evaluate the ability to defecate after surgery. Retrograde urethral X-ray during urination to detect vesicoureteral reflux. Ultrasound to look for CNS, urological, and cardiovascular congenital malformations. If ultrasonography and cystography show abnormalities of the urinary tract, an UIV is indicated. In children who have had a colostomy, have the child perform a contrast-enhanced colonoscopy through the lower colostomy to assess the relationship of the rectal balloon to the coccygeal line or to the sigmoid triangle. and look for a rectal fistula with the urinary or genitourinary tract. In addition, the child will have a pre-anesthetic examination and do tests such as: complete blood count, blood group, coagulation function, urinalysis, kidney function. For children with stoma, conduct enema under the stoma once a day and 1 time before surgery. Children will be given broad-spectrum antibiotics to prevent infection before surgery.
2.2. Steps to perform laparoscopic surgery to lower the ball of the rectum and shape the anus
Children are given general anesthesia, intubation and sacral anesthesia. Next, the child is placed a gastric tube, a urethral catheter. The child's surgical position is supine, with pillows to lift the buttocks, the head is low, the legs are spread and is propped up in the gynecological position. Disinfect the perineum and abdomen from both breasts down.
The surgery usually lasts 90-120 minutes, including two dill laparoscopic and episiotomy.

Phẫu thuật nội soi hạ bóng trực tràng và tạo hình hậu môn
2.2.1. Then laparoscopy
The surgeon will place 3 trocars:
The first 6mm trocar, placed at the navel, for surgical instruments. The second 3mm trocar was placed in the right upper quadrant of the abdomen at the anterior axillary line, for bronchoscopy. The third 3mm trocar was placed in the right lower quadrant of the abdomen at the level of the navel, for surgical instruments. Next, the surgeon will inject CO2 with a pressure of 10-12 cm H2O. A U-shaped nose can be used to hang the bladder over the anterior abdominal wall. Perform rectal dissection up to the fistula. Pair the creepage with 2 clips, then cut the creepage line between the two clips. It is possible to cut and weld the fistula with Ligasure.
2.2.2. Then the perineum
The surgeon uses a nerve stimulator to identify the external anal sphincter. Mark the position of the outer border of the sphincter at 4 positions above, below, on both sides in the shape of a cross.
Then, make a longitudinal incision of 6-9 mm on the anal vestige, creating a tunnel to the anal vestige. Lower the rectal balloon to the anus, observing through the endoscope to avoid torsion of the rectum.
The surgeon removes the clip at the fistula site. Next, suture the rectal wall with the sphincter and the mucosa with the skin, suture the rectum with the anterior fascia, close the umbilical trocar fascia, and sew the remaining 3 trocar holes.
3. Care after laparoscopic rectal balloon lowering and anal shaping
After surgery, give the child pain reliever Paracetamol at a dose of 10-15mg/kg/time x 3 times/day, used for 5-7 days. Use antibiotic Cefotaxime 100mg/kg/day divided into 3 times/day, intravenously, used within 72 hours after surgery. Children are usually discharged after 5-7 days.
Two weeks after surgery, parents will be instructed to start dilating the baby's anus. At the first dilation, parents will use a stick that fits snugly around the anus, dilating twice a day. After each week, the dilatation size will be increased until the baby's rectum reaches the appropriate size.
After the anus has reached the desired size, the doctor will perform surgery to close the stoma. The number of dilations can be reduced when the cane is of the desired size and can be dilated easily without pain to the child. The process of reducing dilatation of each child, parents follow the instructions of the doctor.

Sau phẫu thuật cho trẻ uống Paracetamol theo liều lượng chỉ định
4. Complications may be encountered after laparoscopic rectal balloon lowering and anal reconstruction
Infection of the incision: Give the child antibiotic Cefotaxime 100mg/kg/day divided into 3 times a day. Combined with anal lavage that has just undergone plastic surgery with diluted betadine twice a day. Fistula of the anastomosis: treat by redoing the anastomosis, washing the abdomen in combination with drainage, making an ostomy for the child if not yet. Anal stenosis: Treat by dilating the anus. Intra-abdominal visceral injury due to trocar placement: depending on the extent of the damage, lesions are usually treated laparoscopically. Increased CO2 due to long operative time: treat by increasing ventilation/minute, if the child has hypothermia due to cold and dry CO2, proceed to warm the child. Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in neurological examination and treatment, patients can completely rest in peace. Center for examination and treatment at the Hospital.
To register for examination and treatment at Vinmec International General Hospital, you can contact Vinmec Health System nationwide, or register online HERE.
SEE MORE
Anal dilatation after surgery with narrowing Can anal fistula in children go away on their own? anorectal malformations in neonates