This is an automatically translated article.
Article written by Doctor Le Van Binh - Department of Intensive Care - Vinmec Times City International Hospital
Ventricular septal defect is the most common congenital heart disease with an incidence of about 25% of congenital heart diseases. If not treated properly, ventricular septal defect will cause many effects on the health and development of the child.
1. WHAT IS INTERVARIOUS COMMUNICATION?
Congenital heart disease is quite common in about 0.5 - 0.8% of live births worldwide. Common congenital heart diseases such as ventricular septal defect (CTS), atrial septal defect (CHF), tetralogy of Fallot (F4), and ductus arteriosus (PA), in which the leading cause is CHD accounting for 25-30% .
In Singapore, there are 400 new cases of newborns with congenital heart disease each year. And in Vietnam every year, an average of 16,440 new babies are born with congenital heart disease.
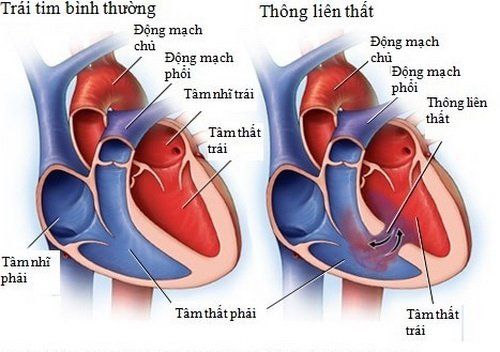
Definition of ventricular septal defect:
There are many different definitions of ventricular septal defect, but in general, there are structural abnormalities of the ventricular septum and hemodynamic disturbances more or less depending on the size of the septum and the flow of the septum. (shunt). There is a structural abnormality of the heart during fetal life with the presence of one or more interventricular septal defects, which may self-close or lead to decreased contractility, requiring or not requiring surgical intervention. . This lesion either alone or in combination causes pulmonary hypertension. Causes of ventricular septal defect
The cause of ventricular septal defect is still unknown. However, people have mentioned a number of factors such as genetics or family: parents or siblings with congenital heart disease, including TLT, have a higher risk of disease. Similarly, children with Down syndrome have a higher risk of developing TLT. If one parent, or both, is addicted to alcohol or drugs, the child is also at a higher risk of developing the disease.
Signs and symptoms of serious heart defects usually appear within the first few days, weeks, and months of a child's life.
Signs and symptoms of a ventricular septal defect in an untreated baby include:
bluish-blue skin, lips, and nails. Eat poorly, do not thrive. Rapid or difficult breathing. Tired easily. Swelling of the legs, feet, or abdomen. Heart beats fast. Although these signs can be caused by other problems, it could be due to a congenital heart defect.
Signs of congenital ventricular septal defect may be seen. If the ventricular septal defect is small, symptoms do not appear until later in childhood. Signs and symptoms vary depending on the size of the ventricular septal defect. The doctor may first suspect a heart defect during regular visits to listen to your baby's heart.
Sometimes a ventricular septal defect is not discovered until adulthood and development of signs or symptoms of heart failure, such as difficulty breathing.
See a doctor if:
Gets tired easily while eating or playing. No weight gain. Becoming short of breath when eating or crying. Blue skin, especially around fingernails and lips. Rapid or difficult breathing. Shortness of breath during light exercise or at rest. Fast or irregular heartbeat. Tired and weak. Swelling in the legs, ankles and feet.

2. IS INTERVARIOUS COMMUNICATION DANGEROUS?
Small ventricular septal defect: Rarely have complications, children live life and develop normally. Complications that can be encountered are endocarditis 1-2%.
Larger ventricular septal defect
Affects cardiopulmonary function, causing many complications such as:
Malnutrition
Malnourished children are more likely to occur when accompanied by heart failure, recurrent infections, and poor diet. Children with malnutrition often lose weight, atrophy the subcutaneous fat layer, when the weight is found to be low weight for age.
Pneumonia
Children can have recurrent respiratory infections, most ominously pneumonia .
Pneumonia is an infection in the lungs, there are many different causes such as bacteria, viruses and parasites ... Clinical manifestations such as fever, cough, shortness of breath, rapid breathing, and contractions. intercostal muscles, chest indrawing, cyanosis (if pneumonia is severe, pneumonia is very severe), children eat poorly, the heart works a lot, so it can easily lead to congestive heart failure, accompanying malnutrition.
Congestive heart failure
Heart failure definition: The heart muscle is no longer able to supply enough to meet the metabolic demands of the body's tissues. Diagnosis when present: + Physical symptoms: Shortness of breath, cough, poor appetite, weak feeding with profuse sweating, little urine.
+ Physical symptoms: Tachycardia, rapid breathing, external auscultation, ventricular septal defect, such as tachycardia, arrhythmia, galloping sound, faint heart sound... Listening to the lungs can detect moist rales in the lungs. 2 at the bottom of the lungs, edema can sometimes be subtle, difficult to detect, hepatomegaly, jugular vein distension, jugular venous hepatic feedback (+)
(older children), Harzer (+).
+ X-ray shows enlarged heart, pulmonary congestion or increased pulmonary circulation.
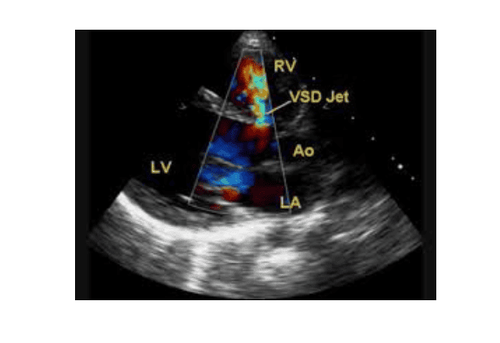
+ Doppler echocardiography: Identify heart failure and heart damage in ventricular septal defect, ventricular and atrioventricular dilatation, valve regurgitation. Importantly, there is impaired left ventricular function with decreased SF and EF.
+ ECG: suggestive of heart disease such as atrial thickening, ventricular thickening, arrhythmia
Heart failure classification has many different authors and cardiovascular associations, such as the American Heart Association of New York, 4 levels heart failure can be applied to children 7 years and older According to Ross classification of heart failure (applicable to young children and older children).
+ Grade I: no activity limitation or no symptoms.
+ Grade II: Dyspnea on exertion in older children. No effects on growth, mild dyspnea or sweating during breastfeeding in infants.
+ Grade III: Difficulty breathing or sweating a lot when feeding or exerting. Prolonged meal time with growth retardation due to heart failure.
+ Grade IV: Symptoms even at rest with tachypnea, involuntary breathing, moaning or sweating.
Infectious endocarditis
Infective endocarditis is one of the possible complications of ventricular septal defect
Definition: Infective endocarditis is an infection of the endocardial surface of the heart . Characteristic lesions are warts of undetermined shape and size. Cause: Mainly streptococcus bacteria, accounting for 55% (Streptococcus viridans and Streptococcus bovis). Staphylococci accounted for 30%, then intestinal bacteria accounted for 6%, rare fungi that cause disease are mainly Candida or Aspergillus. Pulmonary hypertension and islet shunt or Eisenmenger syndrome
Definition: Eisenmenger syndrome is the progression of any left-right shunt (ventricular septal defect) causing pulmonary arterial hypertension to invert right-left shunt Physiology Pathology: Pulmonary artery receives blood from the right ventricle with blood flow from the left ventricle to increase the blood circulation to the lungs, the pulmonary artery system reacts to cause narrowing and increased resistance leading to pulmonary hypertension. . When the systolic pulmonary artery pressure increases > the pulmonary artery pressure then changes the direction of the right-left shunt with cyanosis called Eisenmenger's syndrome or complex. Symptoms: Children have malnutrition, difficulty breathing, poor feeding or feeding, recurrent pneumonia. You can see that the left chest is high and purple. Feel the apex of the heart beating fast and strong, Harzer (+). There is a strong T2 sound in the pulmonary valve fossa, the ATTT gradually decreases or disappears, the ATTT is due to pulmonary valve regurgitation. X-ray: The heart shadow is enlarged, but when the shunt island tends to shrink to near normal, the right ventricle thickens, making the apex slightly rounded and protruding high above the diaphragmatic dome. The pulmonary arch is dilated and dilatation of the two primary pulmonary arteries can be seen, the hilum is hyper-enhanced while the peripheral lung fields are brighter than normal, creating a typical amputation image in the Eisenmenger complex. ECG: Right axis deviation, signs of right ventricular thickening. Doppler echocardiography: Medium and wide opening with pulmonary hypertension depending on the degree, left and right shunt flow. When the pulmonary pressure exceeds the aortic pressure, the right-left shunt flows, the pulmonary artery is dilated, and the right ventricle is very thick.

Some other possible complications
Cardiac arrhythmia: ventricular septum damage affects cardiac nerve conduction, the left and right ventricles are both thickened and dilated, possibly due to progression to heart failure. Clinical diagnosis by palpation and auscultation for bradycardia or tachycardia, regular or irregular, is best confirmed by ECG measurement Cerebral occlusion or brain abscess: possibly due to complications from infective endocarditis or from Eisenmenger syndrome.
3. TREATMENT OF INTERVENTURAL FUNCTIONS
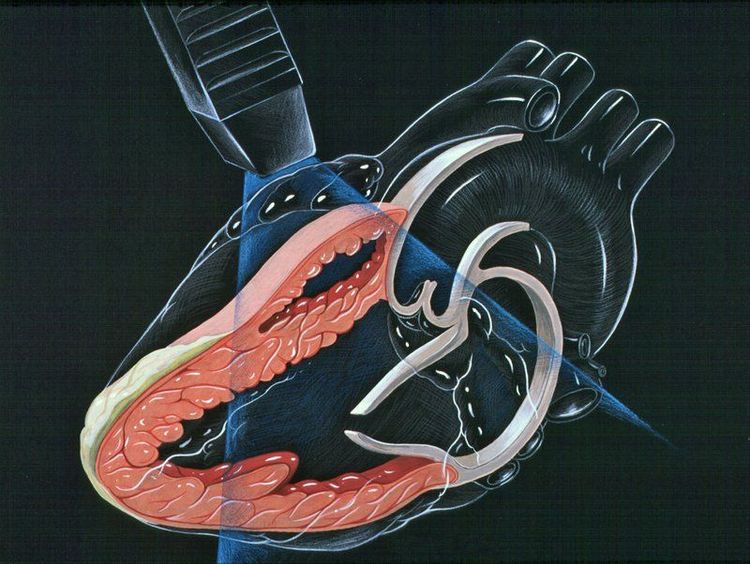
Surgical treatment:
+ Indications: 3 factors related to the time of surgery:
Surgery at neonatal age has a higher mortality rate than at age 1 or 2 The ventricular septal defect can close on its own. Ventricular septal defect with pulmonary hypertension can complicate Eisenmenger complex if the time of surgery is slow. Small ventricular septal defect alone without pulmonary hypertension does not require surgery. Small hole ventricular septal defect (usually ventricular septal defect) but with pulmonary valve regurgitation (Laubry-Pezzi syndrome), even if mild, requires early surgery. Large hole ventricular septal defect with pulmonary artery pressure to systemic pulse pressure >= 0.75 with heart failure not controlled by medical therapy, requiring immediate surgery. Adults with a large ventricular septal defect with pulmonary artery pressure/ALMHT >0.75 but low Qp/Qs due to high pulmonary vascular resistance above 7 units/m2, should not be operated on. * Surgical method:
Surgery to close the ventricular septal defect under the artificial heart-lung machine. It is often necessary to patch the foramen because the conventional suturing method causes damage to the bundle of His and is easy to recur.
* Complications after surgery:
+ Remaining ventricular septal defect.
+ Block right branch.
+ Atrial arrhythmia, ventricular arrhythmia.
+ Existing pulmonary arterial hypertension (in case of delayed surgery).
The ventricular septal defect treatment method at Vinmec International General Hospital has the ability to completely patch the ventricular septal defect to help prevent dangerous complications. With the advantages of the method: helping patients recover quickly, limiting complications and improving the quality of treatment.
If you have a need for consultation and examination at Vinmec Hospitals under the national health system, please book an appointment on the website for service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.