This is an automatically translated article.
The article was consulted with Master, Doctor Nguyen Thi An - Pediatrician - Neonatologist - Department of Pediatrics - Neonatology - Vinmec Ha Long International General Hospital.If patients with congenital hemolytic anemia are not treated early, there will be many complications caused by anemia and iron overload in all organs, changing their appearance. Prevention of hemolytic anemia requires understanding the genetic mechanism, it can be completely prevented.
1. Is thalassemia dangerous?
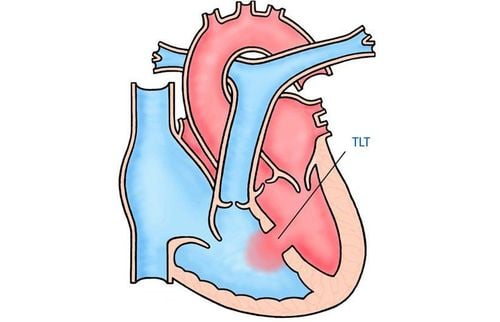
Thalassemia (also known as hemolytic anemia) is a disease with a high rate of congenital diseases. With the main manifestations of anemia and iron overload, patients with thalassemia (congenital hemolysis) need blood transfusions and lifelong iron chelation drugs. With these two measures alone, it is estimated that the treatment cost for a thalassemia patient up to the age of 30 is very expensive (about several billion VND). People with congenital hemolytic disease will have reduced working and living capacity, causing burdens on families and communities.Patients with congenital hemolysis such as short stature, protruding forehead, flat nose, protruding teeth, heart failure, liver failure, endocrine failure....
Thalassemia disease has 2 forms, Alpha-Thalassaemia and Beta- Thalassemia .
Level of expression Congenital hemolytic disease has 5 levels of expression depending on the number of genes damaged:
Very severe, showing fetal edema since in the womb (cases usually cause pregnancy loss before birth). born). Babies can die right after birth due to severe anemia, fetal heart failure. Severe severity manifests as early severe anemia when the child is less than 2 years old. The patient has severe anemia and is early from 5 to 6 months of age. If not detected and treated early, the patient will have severe anemia, jaundice, hepatosplenomegaly. The patient has a distinctive facial expression with protruding frontal bone, protruding occipital bone, protruding maxillary bone, and flat nose. In addition, children are prone to delays in physical, motor and mental development. Moderate levels usually show obvious anemia when the child is older than 6 years. Patients with reduced globin chain, have clinical symptoms of mild or moderate anemia Mild degree, anemia symptoms are often very subtle, patients are often only detected when there are other diseases such as infections, surgery, pregnancy... Usually no normal clinical symptoms or only mild anemia.
2. How long does thalassemia live?
According to an expert of the World Thalassemia Federation, the worrying situation about congenital hemolytic disease is that without treatment, the disease causes death very early from a young age; Inadequate treatment can lead to death at 15 - 20 years of age. However, the cost of treating congenital hemolytic disease is very expensive.Therefore, patient management and disease prevention are urgent issues in order to reduce the rate of birth of children carrying the gene and having congenital hemolytic disease.

Bệnh nhân Thalassemia nếu không được điều trị có nguy cơ tử vong khi chỉ 15 - 20 tuổi
3. Prevention of thalassemia
Avoid giving birth to children carrying 2 disease genes due to being received from both parents by measures such as:3.1. Screening and disease prevention early With pre-marital counseling and testing measures. Couples who are about to become pregnant or are pregnant, especially families who have had Thalassemia patients, should receive pre-marital counseling and diagnosis.
Pre-marital genetic counseling with the goal of birth control between two carriers of the disease. Therefore, before getting married, couples need to be tested to see if they carry the disease gene or not and it is best to avoid marriage between two people carrying the disease gene. Currently, due to the influence of the media, congenital hemolytic disease has been paid much attention and known to many people, so many couples have come to medical centers for advice, avoiding cases when coming to the hospital. The center just discovered that both people carry the disease gene. This has caused a lot of anxiety for the couple.
3.2. Screening for early detection of disease in the fetus Preventing congenital hemolytic disease by screening tests and diagnosing mutated genes during pregnancy. This is an effective and cost-effective measure. If both husband and wife carry the disease gene, the fetus has a 25% chance of having severe disease. In this case, prenatal diagnosis should be done by amniocentesis or chorionic villus sampling and finding genetic mutations. .
Prenatal diagnosis in first trimester pregnant women. In the first 3 months of pregnancy, the mother will have blood drawn for testing to detect abnormalities.

Khám sức khỏe tiền hôn nhân và tiền mang thai giúp sàng lọc phát hiện bệnh sớm
DNA test of 2 parents, mutation of each person. Amniocentesis or chorionic villus biopsies when the mother is pregnant. DNA test of amniotic fluid or placenta. Counseling for termination of pregnancy if the fetus is seriously ill. Using the service of termination of pregnancy (obstetrics) With the above prenatal diagnosis measures, some countries have achieved very good results, even preventing or not giving birth to children with hemolytic disease. heavy organism. This not only limits the difficulties of families with patients, but also gathers resources to provide good treatment for existing patients with hemolytic anemia.
Although traditional prenatal diagnosis methods including amniocentesis and placental biopsy give high accuracy, there are many unsafe factors such as increased risk of miscarriage, amniotic fluid leakage, vaginal bleeding. , infection, ... Traditional screening methods including maternal serum screening (double test, triple test) and ultrasound have not yet met the wishes of pregnant women because of the high false-positive rate. increase the rate of pregnant women having unnecessary amniocentesis.
One of the methods being implemented at Vinmec International General Hospital to screen for fetal malformations as well as thalassemia is the non-invasive screening method NIPT.
During pregnancy, in the mother's blood, in addition to her own DNA, there is also the free DNA of the fetus. Instead of amniocentesis, which has a direct effect on the fetus, the non-invasive prenatal screening method (NIPT) is much safer because only 20ml of blood is taken from the mother's vein from the 9th week of pregnancy onwards. Go to DNA sequencing. This result will help experts detect fetuses with high risk of abnormalities of some chromosomes such as Down syndrome, Patau, Edward, Turner, Thalassemia, ...
At the same time reduce the rate pregnant women with unnecessary amniocentesis. The outstanding advantage of this method is that it is non-invasive and can be carried out as early as the 9th week of pregnancy. Older pregnant women, families with children with birth defects... should choose NIPT from early pregnancy.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.