This is an automatically translated article.
The root canal procedure of the incisors is essentially the removal of the entire pulp that has been damaged by bacteria. Along with that, the doctor will clean the gaps and fill them with specialized dental materials. So is root canal treatment painful? How long does root canal treatment take? The following article will help you better understand about root canal treatment.1. Structure of teeth and causes of pulp infection
1.1. Structure of teeth
The crown is the protrusion above the gum line. The part across the gum line is called the neck, and the part below the gum line is the root. The root can be twice as long as the crown.A root can split into two canals, which means that each tooth usually has a maximum of four canals. In rare cases, six or seven roots have been found in a molar.
The hard white coating on the outside of the crown is called enamel. This is the part you need to protect by brushing and flossing every day. The accumulation of bacteria on teeth due to poor oral hygiene can lead to tooth decay.
If tooth decay eats away even a small amount of enamel, it leaves the rest of the tooth vulnerable to infection. Once bacteria begin to eat away at the soft pulp inside the tooth, it can rapidly spread down the root(s) through the root canal system. From here it can reach the surrounding bone and gum tissue.
Untreated pulp infection has the potential to lead to an oral abscess.
1.2. Causes of marrow infection
A pulp infection can occur for a number of reasons, although the underlying root of the problem has always been bacterial colonization of the pulp. The reason for the infection of the pulp is determined to be due to the way the bacteria get into the pulp. In this paragraph, we list the main causes of such infections. Reasons for tooth infection include:Cavities allow bacteria to enter the pulp and cause infection. Cracked or damaged teeth, opening the way for bacteria. Various tooth displacements due to extrusion, infiltration or compression. Aseptic necrosis due to tooth trauma (signs include tooth discoloration or highly calcified canals, which can be identified by X-ray). Abnormal dental anatomy allows bacteria to infect the pulp tissue. Repeated dental treatment on the same tooth. According to the experience of dentists, the main cause of pulpitis is tooth decay that damages the teeth, creating conditions for bacteria to enter and infect the pulp. This is why it is important to identify and remove tooth decay promptly to prevent infection of the pulp.
2. Symptoms of incisor pulp infection
2.1. Pain
Strong pain does not always mean that a patient needs root canal treatment. In some cases, the tooth that needs surgery may not even be painful. However, when pain is present, this may indicate the need for a root canal. By determining whether the pain is intense and sharp or a dull ache, patients can understand what to expect during their next dentist visit.Types of pain that can help identify a pulp infection include:
Pulsating toothache; Pain intensity changes as the patient changes position; The pain is so severe that the patient cannot sleep at night. Spontaneous toothache (continuous or intermittent); Pain caused by specific stimuli such as percussion, pressure or heat insult (eating hot food immediately after cold food and vice versa); The toothache cannot be completely eliminated with pain relievers; The patient can easily identify which tooth is in pain, or indicate the area of pain. So any kind of pain can be a sign that the pulp is infected and requires corresponding treatment. Pain must be considered along with other symptoms to indicate a problem.
2.2. Swelling
Swelling does not always indicate a need for root canal surgery. Even so, when it is present along with any kind of toothache, it may indicate the need for such treatment. Swelling can come in many different forms and types. Whether it looks normal with some kind of pain or is a clear lump that can be easily seen or palpated, it usually means that root canal surgery is needed. In some cases, the swelling may even spread to the patient's face or neck.Swollen features that may indicate a pulp infection include:
Swollen gums located in front of the root apex. Fistula at the tip of the tooth Visible swelling can be of any size: from barely visible to a clearly palpable lump. Swelling can last several days or months. Bad breath is caused by pus coming out of the canal. The problem tooth has a higher sensation than the neighboring teeth. Swelling may not be accompanied by a toothache, but it still means a root canal is needed. Furthermore, swelling itself is not always a sign that you need such a procedure; However, swelling is always a sign that the tooth needs urgent medical treatment. In most cases, dentists prescribe oral antibiotics to deal with the infection and eliminate swelling.
3. Is the root canal treatment painful?
Infected pulp usually develops quite slowly, from untreated tooth decay to pulpitis. When a tooth has undergone many restorations, or when a crown or filling is loose or faulty, the chance of a root infection is higher. In some cases, an infection can develop more quickly, such as if you have an injury or a cracked or chipped tooth.If you have regular dental exams, your dentist will be able to identify and treat any decay before it enters the root system. However, if you haven't been to the dentist for a while, you may find that the infection has spread and you need root canal treatment to save the tooth.
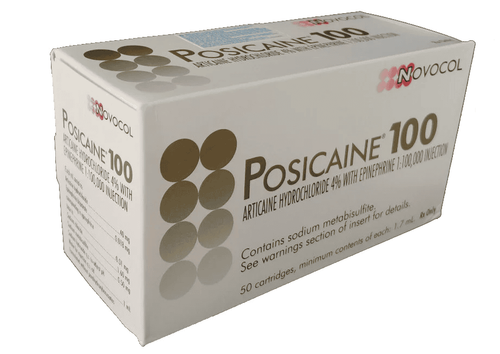
Root canal treatment is a fairly simple minor surgery, not invasive to the gums or jawbone. However, discomfort during the procedure is inevitable. But you do not need to be too worried because everything is within the limits of human tolerance and dentists will have a solution to help their patients undergo minor surgery in the most gentle way. Using this device works based on the mechanism of creating vibration waves that block pain transmission to the brain to help neutralize the feeling of numbness when numbing. When the anesthesia is divided, the manipulations take place smoothly as if there is no impact on the teeth to give the patient the most comfortable feeling as well as the best psychology for the procedure to be conducted smoothly.
If you are still unsure, it is advisable to discuss with your dentist before starting any work and possibly “additional” for a longer period of treatment. Before your treatment, you can tell your dentist that you will raise your hand if you start to feel uncomfortable at any point.
Special neurological patients can opt for intravenous sedation while the job is completed.
4. The process of taking root canal in front teeth
Visit: After listening to your symptoms and concerns, your dentist will use expert methods to determine if endodontic treatment is needed. Methods dentists use to indicate a need for a root canal include: X-Rays: Dentists use x-rays to determine radioactivity, which is a term that identifies a dark spot on the tip of a problem tooth, and indicated that the bone change had occurred due to an infection inside the tooth. Identify persistent or recurrent gingival boils: Boils are essentially pus-draining fistulas that help pus drain out instead of seeping into the soft tissues around the tooth. So the pus will find a way out: It can get into the soft tissues and cause swelling, or it can create a drain to go outside. If the drain is blocked, pus can cause swelling. Such areas are usually tender to the touch, but they do not necessarily indicate a need for a root canal. In some cases, such damage can also be caused by gum disease (periodontal problems). Identify problem teeth that are darkened: Discoloration of teeth means that some change has occurred in the neural space. In many cases, this sign indicates the need for root canal treatment. Discoloration usually occurs as a result of some type of tooth trauma, in some cases taking up to 10 years for the discoloration to appear. Furthermore, the discoloration may not be accompanied by toothache or swelling. However, a darkened tooth is not always a sign that endodontic treatment is needed. This symptom is often paired with others to determine the course of treatment needed. Nerve Exposure: Because it is difficult to determine how the nerve is located with the tooth surface, contact of this nerve can occur if the dentist comes into contact with pulp tissue during the procedure. treatment. In this case, a root canal should be obtained, as exposure can cause tissue degeneration in the future. Knock on the problem tooth. Procedure: Step 1: Anesthesia At this stage, the specialist will administer a local anesthetic to eliminate any pain the patient may be experiencing. Despite the fact that the inner nerve usually dies in these cases, the dentist may still administer anesthesia to eliminate any pain that may be present. Step 2: Place the Dentistry The dental implant is a rubber sheet to ensure a dry area around the problem tooth. This dam prevents saliva from reaching the treated area. Step 3: Create an opening and remove the infected pulp. Using a drill, your dentist will make a hole in the top of your tooth (or in the back of your front tooth) through which they can access pulp chamber and root system. Tiny files are used to remove damaged and dead pulp and nerve tissue from inside the tooth and root. Root canals are very thin and often curved, so it may take some time for the dentist to locate all the canals and make sure to remove all traces of infected material. They often use special microscopes and lights to help them see just inside the tooth. If you have an abscess at the end of the root, it will now be drained. Since the procedure is under anesthesia, the procedure is painless. After the hole is made correctly, the inside of the tooth is cleaned with water and an antibacterial solution. The dentist uses a syringe to suck the cleaning solution into your teeth, which is then sucked back out. This is repeated several times to make sure the area is completely sterile. Step 4: Apply medicine to the gap In case your tooth has an internal infection, the dentist will apply medicine to the inner tooth area to remove bacteria. Your tooth may then be filled with a temporary filling until you return at your next visit. In some cases, the hole may be left open until the next visit, allowing the pus to drain out. Step 5: Filling At this stage, your dentist will seal your teeth. They first replace the temporary material inside your tooth with a permanent replacement, and then seal the filling. Step 6: Restoration In the final stage, your dentist will completely restore your treated tooth. In many cases, because teeth are more prone to fracture after root canal treatment, your dentist may recommend a root canal and crown. A crown (also known as a 'hat') is a protective layer usually made from porcelain or metal. It covers the entire tooth to protect the tooth from further damage. To fit a crown, your dentist must first scrape off some of the enamel on the outside of your tooth. They use strong dental glue to keep it in place. Once fixed in place, it will feel and act like natural teeth. Of course, the cost of root canals and crowns is higher than root treatment alone, but your dentist will tell you what is best for the condition of your teeth. Your dentist may wait a few weeks before placing your crown, just to be sure the process was successful and that there are no signs of infection after the root canal has been filled.5. Pros and cons of root canal therapy
Since there is no more effective method to remove a pulp infection, endodontic surgery is far more beneficial than extraction or ignoring the problem in general. However, this type of treatment also has some unavoidable disadvantages. The dangers and discomforts of the pulp are actually the price to pay to save your tooth.Advantages When performing treatment, patients will no longer feel pain and do not need to take pain relievers to eliminate sensitivity caused by problem teeth. Because bacteria are removed as part of root canal therapy, the spread of any internal infection should be prevented. This treatment helps prevent the formation of an abscess around the apex of the problem tooth. Root canal treatment will not have a negative impact on the sensation or force of your bite. Problem teeth will only need a few days to recover. Such treatment allows you to preserve your own tooth and retain the natural ability to chew. Applying root canal therapy allows you to protect adjacent teeth from stress. Saving your own tooth helps you avoid spending money on expensive artificial crowns and implants, or being embarrassed about any missing teeth. Cons After root canal treatment, patients may experience discomfort or even minor pain for the first few days. Pain relievers can help with the coping process. The treatment can lead to discoloration of the problematic tooth. Immediately after treatment, the tooth is weak, which is why it is recommended to avoid actions such as chewing, until it is completely restored by the dentist. Unfortunately, the treated tooth will lose its original strength and strength after the infection and treatment results. It is not possible to get 100% clean tooth pulp. The infection may reappear if the final recovery is not completed in time. Using inexpensive materials of low quality may result in having to repeat additional treatments in the near future. An extra or hidden canal will force you to have the treatment done again.
6. Taking care of teeth after taking the pulp
Once your procedure is done, your endodontist will give you strict aftercare instructions that you need to follow. You should always first follow the following care instructions from your endodontist, but the general rules are as follows:Take the pain reliever as directed Fasting until the numbness in the mouth is gone Do not bite or chew with your treated front tooth until it is fully restored Brush and floss daily as usual You may feel some mild pain and soreness after the procedure, and the pulp recovery period can last a week or two. However, make sure to contact your endodontist as soon as possible if you experience:
Sharp pain after root canal: If you have sharp or severe pain after root canal, even Once you've taken pain medication, it means you've had an unsuccessful root canal and you should call your dentist right away. Swelling after a root canal: Some swelling and pain are normal after a root canal and should go away after a few days. If it doesn't, or the pain gets worse, call your dentist. Toothache after root canal when biting: Some discomfort, pain or sensitivity is normal after having your pulp removed. However, if you continue to feel pain when biting down, it may be because your flap is not flattened enough. If that's the case, you should call your dentist to fix it because not paying attention to the problem can make things worse. Toothache months after a root canal: Your tooth may not heal properly after a root canal, or it may have a new fracture or decay. If you have pain a few months later, you should call your dentist. Jaw pain after root canal: It's normal to feel pain in your jaw, if it doesn't go away or gets worse, you need to call your dentist. Allergic reaction to your medication An uneven bite A temporary tooth crown or your filling falling out Infection after root canal: Severe pain that gets worse a week after the procedure could be a sign of an infection, and you should call your dentist. The same symptoms you had before the root canal
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.