This is an automatically translated article.
In fact, insulin resistance may actually be at the root of a person's polycystic ovary syndrome (PCOS), playing a role in causing the condition in the first place, as well as in exacerbating symptoms. its evidence. Insulin resistance requires management with lifestyle changes or drug treatment to prevent complications, so every woman with PCOS should be screened. Read more below to understand insulin resistance and PCOS.1. Polycystic ovary syndrome (PCOS): Symptoms, causes and treatment
Up to 30% to 40% of women with polycystic ovary syndrome (PCOS) also have insulin resistance — a condition that leads to high blood sugar and potentially prediabetes and type 2 diabetes. Polycystic ovary syndrome (PCOS) is a condition that affects a woman's hormone levels. Women with PCOS make higher than normal levels of male hormones. This hormone imbalance causes their bodies to mess up in their menstrual cycles and make it harder to get pregnant.PCOS also causes hair growth on the face and body as well as baldness . It can also contribute to long-term health problems, such as diabetes and heart disease. Birth control pills and diabetes medications (against insulin resistance, a PCOS symptom) can help correct hormone imbalances and improve symptoms.
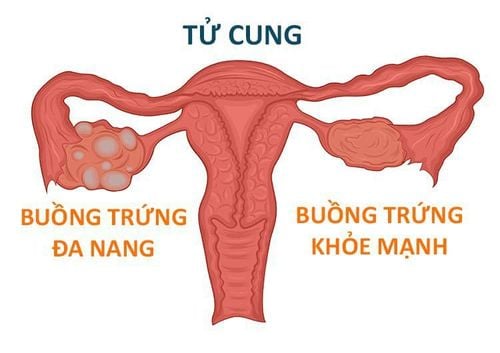
1.1. What is Polycystic Ovarian Syndrome (PCOS)? PCOS is a problem with hormones that affects women of childbearing age (ages 15 to 44). Between 2.2 and 26.7 percent of women in this age group have PCOS. Many women have PCOS but don't know it. In one study, up to 70% of women with PCOS went undiagnosed. PCOS affects a woman's ovaries, the reproductive organ that produces estrogen and progesterone, the hormones that regulate the menstrual cycle. The ovaries also produce small amounts of male hormones called androgens. The ovaries release an egg to be fertilized by a male sperm. Ovulation every month is called ovulation. Follicle-stimulating hormone (FSH) and luteinizing hormone (LH), produced in the pituitary gland, control ovulation. FSH stimulates the ovaries to produce a follicle - a sac that holds an egg - and then LH triggers the ovary to release a mature egg.
PCOS is a “syndrome” or group of symptoms that affect the ovaries and ovulation. The three most common symptoms of this condition are:
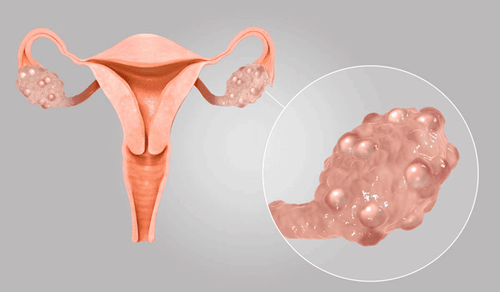
Cysts in the ovaries Elevated levels of male hormones in the body Irregular periods or even missed periods In PCOS, many small sacs are filled with fluid develop inside the ovary. The word “polycystic” means “many cysts”. These sacs are actually follicles, each containing an immature egg. The egg will never mature enough to trigger ovulation. The lack of ovulation alters the levels of estrogen, progesterone, the hormone FSH, and the hormone LH. Progesterone levels are lower than normal, while androgen levels are higher than normal.
Additional male hormones disrupt the menstrual cycle, so women with PCOS have less menstrual periods than usual. PCOS is not a new disease. An Italian doctor named Antonio Vallisneria first described its symptoms in 1721.
Có tới 30-40% phụ nữ mắc hội chứng buồng trứng đa nang
Heredity
Studies show that PCOS often runs in families with a history of the condition. Scientists think genes - not one but many genes contribute to this syndrome
Insulin resistance
Up to 70% of women with PCOS have insulin resistance, meaning their cells can't use it insulin properly.
Insulin is a hormone produced by the pancreas to help the body use sugar from food for energy. When cells cannot use insulin properly, the body's need for insulin increases. The pancreas will make more insulin to compensate. The extra insulin will trigger the ovaries to produce more male hormones. Obesity is the main cause of insulin resistance. Both obesity and insulin resistance can increase the risk of type 2 diabetes.
Inflammation
Women with PCOS will often have increased levels of inflammation in their body. Being overweight can also contribute to inflammation. Studies have linked excessive inflammation with elevated androgen levels in a woman's body.
1.3. Common symptoms of polycystic ovary syndrome Some women begin to see symptoms of PCOS around the time of their first period. Others only find out they have PCOS after they've gained a lot of weight or they've had trouble getting pregnant. The most common PCOS symptoms are:
Irregular menstruation. The lack of ovulation prevents the lining of the uterus from ovulating every month. Some women with PCOS have fewer than eight periods a year or even no periods at all. Excessive bleeding. The lining of the uterus forms over a long period of time, so menstrual symptoms in women with PCOS may be more severe than usual. Lots of hair growth. More than 70% of women experience hair growth on the face and body - including on the back, abdomen and chest. Acne. Male hormones can make the skin oilier than usual and cause breakouts on areas like the face, chest, and upper back. Weight gain. Up to 80% of women with PCOS are overweight or obese. Male pattern baldness. Hair on the scalp is thinner and may fall out. Dark skin. Dark patches of skin can form into wrinkles on your body such as on your neck, in your groin, and under your breasts. Headache. Hormonal changes can cause headaches in some women. 1.4. Treatment of polycystic ovary syndrome Birth control pills and certain other medications can help regulate your menstrual cycle and treat PCOS symptoms like hair growth and acne.
Using birth control pills
Taking a progestin daily can:
Restore a normal hormone balance Regulate ovulation Reduce symptoms like excess hair growth Protect against endometrial cancer These hormones can in a pill, patch, or vaginal ring.

Kinh nguyệt không đều là triệu chứng điển hình của hội chứng buồng trứng đa nang
Metformin (Glucophage, Fortamet) is a medication used to treat type 2 diabetes. It also treats PCOS by improving insulin levels. One study found that taking metformin in combination with making dietary changes and exercise improved weight loss, lower blood sugar, and restore a normal menstrual cycle better than taking metformin. Just change your diet and exercise.
Clomiphene
Clomiphene (Clomid) is an assisted reproductive medicine that can help women with PCOS get pregnant. It is important to note that when you are discussing family planning, keep in mind that clomiphene increases your chances of having twins and having more children
Hair removal
A few treatments that can help get rid of it unwanted hair or prevent hair growth. Eflornithine (Vaniqa) cream is a prescription medication that will slow hair growth. Laser hair removal and electrolysis can help remove unwanted hair from your face and body
Surgery
Surgery may be an option to improve fertility if treatments otherwise ineffective. Ovarian drilling is a procedure that makes small holes in the ovaries with a laser or thin heated needles to restore normal ovulation.
2. Insulin resistance and polycystic ovary syndrome PCOS
2.1. What is insulin resistance? Under normal conditions, the hormone insulin rises shortly after eating. It stimulates the liver and muscles to absorb sugar from the blood and convert it to energy. That then causes blood sugar to drop, and then insulin to drop. With normal insulin sensitivity, both sugar and insulin are normal on a fasting blood test. With insulin resistance, blood sugar can be normal, but insulin is high. Because the pancreas has to make more and more insulin to try to get its message across. Too much insulin creates inflammation and causes weight gain. It can also lead to type 2 diabetes and heart disease. Too much insulin is also an underlying physiological driver of polycystic ovary syndrome.2.2. Relationship between insulin resistance and PCOS Insulin resistance is a key feature of obese and lean PCOS. It occurs in 70-95% of people with obese PCOS and 30-75% of people with lean PCOS. High insulin isn't just a symptom of PCOS — it's also a major cause of the condition. High insulin can decrease ovulation and cause the ovaries to make excess testosterone.
One study observed that increasing rates of PCOS correlated with an increase in obesity and weight gain over the past ten years. Another paper describes “a galloping increase (of PCOS) paralleling an increase in type 2 diabetes”.
2.3. Insulin resistance test To determine insulin resistance, it is essential to confirm insulin resistance with a blood test such as fasting insulin, HOMA-IR index, or a 2-hour insulin challenge test. By testing for insulin resistance, doctors can identify PCOS patients who don't have insulin problems, such as a small group with adrenal PCOS and a sizable group with a misdiagnosed hypothalamic amenorrhea. is “thin PCOS”.
2.4. Conventional Treatment for Insulin Resistance and PCOS Conventional treatment recommendations for the insulin resistance aspect of PCOS include weight loss, aerobic exercise, and the diabetes drug metformin, which improves insulin sensitivity. Resistance training may also be effective, but more research is needed.
Oral contraceptives are the other officially recommended treatment for PCOS, but they can interfere with the sugar regulation and insulin resistance that underlie PCOS. The link between PCOS, insulin resistance, and oral contraceptives is considered a "conundrum of modern medicine" and requires further investigation.
2.5. The role of fructose in insulin resistance For patients with polycystic ovary syndrome, the most effective dietary intervention is to reduce fructose intake.
Fructose itself is not a problem, only in large amounts can it be harmful. For example, low-dose fructose from fruit does not cause insulin resistance and is instead beneficial for insulin sensitivity and health. High doses of fructose from desserts, soft drinks and juices have a very different effect. One researcher explains: “There is a fundamental physiological difference in how smaller and larger amounts of sugar are processed in the body. At high doses, fructose can crowd out normal processing pathways in the small intestine and possibly reach the liver, where it can cause inflammation and decrease insulin sensitivity.

Kháng insulin xảy ra ở 70-95% phụ nữ PCOS béo phì
Magnesium is the second most recommended supplement after inositol for insulin resistance because it corrects the common subclinical magnesium deficiency that some researchers suspect may contribute to resistance. insulin and heart disease. Magnesium deficiency affects at least a third of people, and possibly more, and cannot be easily or reliably diagnosed with a blood test. A recent meta-analysis concluded that magnesium supplementation is effective for treating insulin resistance in people with magnesium deficiency, and one small study found that concomitant supplementation of magnesium, zinc, calcium, and vitamin D improve insulin metabolism of PCOS patients.
The majority of people with polycystic ovary syndrome (PCOS) have insulin resistance or high insulin. High insulin is both a symptom of PCOS and an underlying physiological driver. Testing for insulin resistance can be helpful to rule out other conditions that are often misdiagnosed as PCOS. Polycystic ovary syndrome (PCOS) sounds like it's just a disease of the ovaries, but it's not. Although PCOS affects the ovaries and ovulation, it is actually a whole body metabolic and endocrine disorder that is closely related to insulin resistance.
If you have a need for consultation and examination at Vinmec Hospitals under the national health system, please book an appointment on the website (vinmec.com) for service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: helloclue.com, virtahealth.com, healthline.com, msdmanuals.com