This is an automatically translated article.
The article is professionally consulted by Specialist Doctor II Nguyen Thai Hung - Ophthalmologist - Department of Medical Examination & Internal Medicine - Vinmec Danang International General HospitalA corneal transplant is a surgical procedure to replace part of a patient's cornea with corneal tissue from a donor. The condition to receive the cornea is when the patient has damaged cornea and is close to the age of the donor. So what are the conditions and indications for corneal transplant?
1. What is a corneal transplant?
The cornea (iris) is a transparent tissue that occupies 1/6 of the eyeball area and is located in front of the eyeball shell. The cornea is like a lens with a thickness of about 0.5mm at the center and about 1mm at the periphery to help focus light into the eye so you can see. The cornea is made up of 5 layers of cells. These layers work together to protect your eyes and provide clear vision.Your cornea must be transparent, regular, and smooth to have good vision. If it is scarred, edematous, or otherwise damaged, light is not properly focused on the eye. As a result, your vision is blurred or you see bright lights.
If your cornea is incurable, causing permanent irreversible damage, your eye doctor may recommend a corneal transplant. This is when the diseased cornea is replaced with a healthy cornea from a donor. The cornea can be received after the donor has passed away, between 6 and 8 hours after the death.
A donor is someone who chooses to donate (donate) his or her corneas after they die to people who need them. All donated corneas are carefully tested to make sure they are healthy and safe to use. Anyone can donate a cornea after death, usually regardless of age or sex. In particular, people who have received a corneal transplant can also donate it when they die. Cornea after harvesting can be preserved for 14 days. However, the sooner the transplant the better
This is a highly successful surgery: When performed by an experienced corneal surgeon, the 10-year graft survival rate is more than 90 % and the average lifespan of the graft is about 15-20 years.
Only about 15% of people with keratosis need to consider a corneal transplant. That number is dwindling with the advent of collagen crosslinking in the cornea to prevent the progression of the apical cornea and more advanced, specialized contact lens designs for the apical cornea.
Corneal transplantation is a life-changing procedure and patients with apical keratosis should consider a corneal transplant until they have exhausted contact lens options. These contact lenses need to be fitted by a specialized contact lens specialist.
Cases of corneal transplant: Usually, when you have eye problems, you will visit an eye clinic and be examined by an eye specialist. Here, they will carefully examine and evaluate and grade the damage of the cornea, as a basis for the indication for transplantation.
The condition of the patient's cornea before receiving the transplant is very important for the prognosis of the transplant: Patients with hereditary corneal dystrophy (Fuchs) problems, cone-shaped corneas (Petular cornea), or corneal scars with less neovascularization... have a better surgical prognosis than preoperative patients with thick neovascular scars, severe infections that damage the posterior part of the eyeball,... or in patients with comorbidities such as glaucoma, dry eye due to allergies, ... or diseases that still cause continued damage to the cornea have not been definitively treated.
The age of the patient is equally important: The operative prognosis and postoperative course in younger patients are generally milder and better than in the elderly. Therefore, the order of priority selection for transplants with good prognosis will have a higher successful outcome.
2. Corneal transplant surgery options
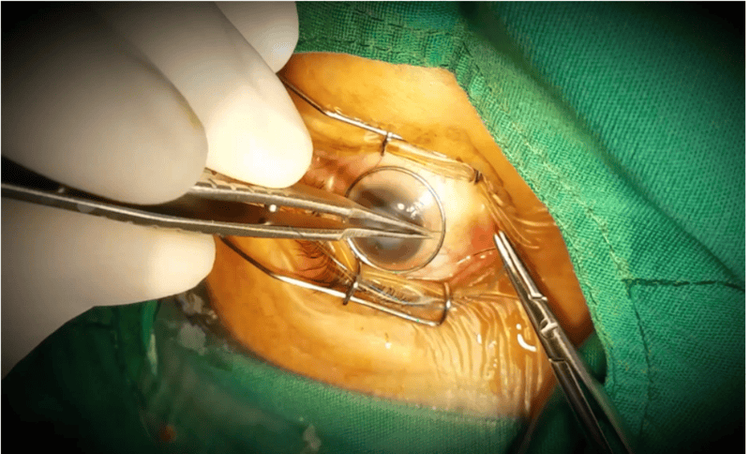
2.1. Full-thickness corneal transplant Your entire cornea may need to be replaced if both the front and inner layers of the cornea are damaged. This is called a penetrating corneal transplant (PK), or full-thickness corneal transplant. Your diseased or damaged cornea will be removed. The clear donor cornea is then stitched into place.PK has a longer recovery time than other types of corneal transplants. It can take up to a year or longer to regain complete vision after PK.
With PK, there is a slightly higher risk than with other types of corneal transplant that the cornea will be rejected. This is when the body's immune system attacks the new corneal tissue.
2.2. Partial thickness corneal transplant Sometimes the anterior and middle layers of the cornea are damaged. In this case, only those layers will be removed. The endothelium, or thin dorsal layer, is held in place. This implant procedure is called anterior deep keratoplasty (DALK) or partial thickness corneal transplantation. DALK is commonly used to treat keratosis or bulging of the cornea.
The healing time after DALK is shorter than after a whole corneal transplant. There is also less risk of new cornea being rejected.
2.3. Keratosis endothelial layer In some eye conditions, the innermost layer of the cornea called the "endothelial" is damaged. This causes the cornea to swell, affecting your vision. Endothelial keratoplasty is a surgery to replace this layer of cornea with healthy donor tissue. It is called a partial transplant because only this inner layer of tissue is replaced.
There are several types of endothelial stratum corneum. They are called:
DSEK (or DSAEK) - Descemet's endothelial (automatic) keratoplasty. DMEK - Descemet's Membranous Endothelial Keratoplasty. Each type removes damaged cells from an inner layer of the cornea called the Descemet membrane. The damaged corneal layer is removed through a small incision. Then the new tissue is put in place. Only a few stitches are needed to close the incision. Most of the cornea is left intact. This reduces the risk of rejection of new corneal cells after surgery.
Some things to know:
With DSEK/DSAEK surgery, donor tissue can be easier to transplant and localize because it is thicker than donor tissue in DMEK surgery. In DMEK surgery, the donor tissue is thin and can be more difficult to transplant. However, the recovery is faster because the implant is thinner. Your eye surgeon will choose the type of surgery based on the condition of your cornea.
3. Things to note
3.1. A few days before surgery Your eye doctor will explain to you about corneal transplant surgery. You will discuss why you need this surgery, how it can help you see better, and what you can expect during and after surgery.When surgery is indicated, the doctor will admit you to the hospital and wait for the day of the transplant. That date may change if a good donor cornea is not ready for you by that time.
Tell your eye doctor about all the medicines you take. They will let you know if you can continue taking them before surgery.
You may need to stop taking your anticoagulants before surgery and have additional tests done. This is to ensure that you are healthy enough to undergo transplant surgery.
3.2. After the transplant The day after your corneal transplant surgery, you will have to return to the ophthalmology clinic for an eye exam.
Stitches from surgery may or may not require removal. This depends on how long you heal, the health of your eye, and the type of sutures used.
As you recover from surgery, here's what you need to do to take care of your eyes:
Use eye drops exactly as prescribed by your eye doctor. Do not press or rub your eyes. If necessary, take an over-the-counter pain reliever. Ask your doctor which ones you can take. Wear sunglasses or an eye shield to protect your eyes. Talk to your eye doctor about when you can return to your normal daily routine. Depending on your implant, you may need to lie on your back for a while after surgery. This keeps the new donor tissue in place. Call your eye doctor if you have concerns or questions about how to take care of yourself at home.
Depending on the type of implant you've had and how your eye heals, it may take a year or more to fully recover from this surgery.
3.3. Possible problems with corneal transplant Organ rejection is when the body's immune system sees the transplanted tissue as something it shouldn't be and tries to get rid of it. Rejection is a problem for 3 out of 10 people who receive full-thickness (PK) implants. Risks are lower with partial thickness surgery.
Warning signs that your body is trying to refuse your corneal transplant include:
Eye pain Extremely sensitive to light Red eyes Cloudy or hazy vision Tell your eye doctor you right away if you have any of these signs.
Sometimes a corneal transplant can cause other eye problems such as:
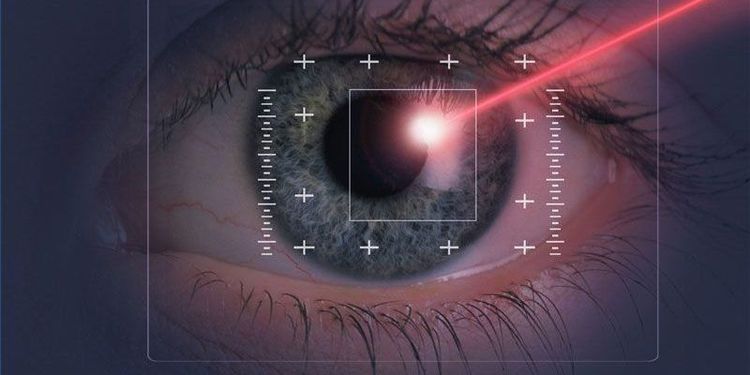
Infection Bleeding Detached retina (where tissue lining the back of the eye pulls away from the eye) Glaucoma (caused by increased pressure inside the eye) in the eye) Even if the corneal transplant works as it should, other eye problems can limit the quality of your vision. For example, the new cornea may not curve as often (called astigmatism). Or you could have an eye disease like macular degeneration, glaucoma, or diabetic retinopathy.
Some people may need more than one corneal transplant. The first transplant may be rejected or other problems may occur. However, a repeat transplant has a higher rejection rate than the first transplant.
To examine and treat eye diseases, you can go to the Eye specialist - Vinmec International General Hospital. The department has a comprehensive vision and eye health care function for children, adults and the elderly including refractive error testing, general examination, diagnostic ultrasound, laser treatment and surgery. In addition, ophthalmology also has the task of coordinating with other clinical departments in the treatment of pathological complications and eye injuries caused by accidents.
Why should you choose to examine and treat eye diseases at Vinmec International General Hospital?
Simple and quick procedure. Enthusiastic advice and support, reasonable and convenient examination process. Comprehensive facilities, including a system of clinics and consultations, blood collection room, dining room, waiting area for customers... The medical staff has high professional qualifications, style. Professional, caring way of working.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: corneal apex.org.au