This is an automatically translated article.
The article is professionally consulted by doctors working at Oncology Center - Vinmec Central Park International General HospitalThe immune system is considered as a barrier to protect the body from pathogens, especially in cancer. Therefore, leveraging and stimulating the body's immune system is an important key in controlling cancer and increasing patient survival. Immunotherapy stimulates the immune system to fight cancer cells in a variety of ways without the use of other interventions such as surgery, chemotherapy, or radiation.
1. The Immune System's Role in Cancer and Cancer Multidisciplinary Treatment
1.1. Cancer and the Immune System: A Dynamic Relationship
The immune system plays an important role in the human body through its defense mechanisms against foreign agents such as viruses or microorganisms. The immune system is considered as a barrier to protect the body from pathogens, especially in cancer. However, an irony is that most types of cancer cells have the ability to evade the immune system, so tumor cells are increasingly growing and can metastasize to any organ in the body. . Many scientific studies show that when the patient's immune system is weakened, the risk of cancer increases. Therefore, utilizing and stimulating the body's immune system is an important key in controlling cancer, preventing disease progression and increasing patient survival. Treatment with the body's natural immune system (or Immunotherapy) is considered a fourth cancer therapy after surgery, chemotherapy, and radiation therapy.Immunotherapy is a method of treating cancer by stimulating the patient's immune system to fight cancer cells in different ways without using other intervention methods such as surgery. surgery, chemotherapy, radiotherapy. 3 Immunotherapy has been studied and clinically tested for more than half a century with many achievements. However, understanding the human immune system remains a major obstacle in drug research and development of clinically applicable therapies.
1.2. Natural Immune Response and Characteristics of an Effective Immune Response
Antigen presenting cells (APCs) are specialized cells that can recognize foreign antigens and present these antigens to T-cell lymphocytes. Antigens are molecules produced by foreign microorganisms that attack the body, these antigens are attached to T cells and antibodies. The association between antigen-presenting cells and T cells helps to activate T cells. The activated T cells then divide rapidly and begin to attack foreign antigen-containing agents.There are many important characteristics of an effective immune system that can help the body fight harmful agents. These important characteristics include specificity, blood fluidity, adaptability, and persistence (ability to remember harmful agents). Among them, the most important feature is specificity to ensure that the immune response will target the cancer cell's antigen. A simple example of the specificity of the immune system is in type 1 diabetes (an autoimmune disease). When the patient has the disease, the T cells recognize and destroy the beta cells responsible for insulin production in the lobules of Langerhans of the pancreas, while this phenomenon is difficult to observe in other lobes.
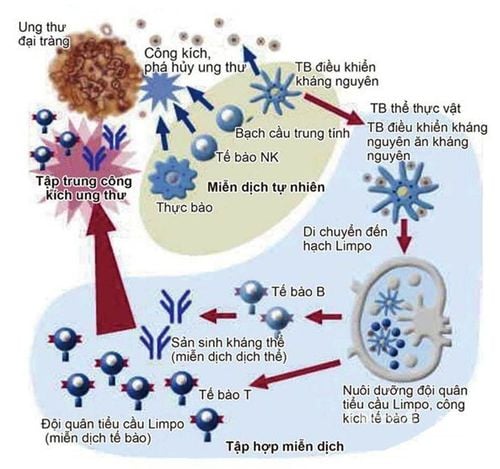
Tập hợp miễn dịch.
1.3. Role of Immunotherapy in Cancer Multidisciplinary Treatment
Multimodal therapy or Holistic Therapy was first mentioned by oncologist Pierre Denoix as a combination therapy with specialized therapeutic modalities such as surgery, chemotherapy, and radiation. used throughout the course of the disease. Multimodality treatment is considered as a comprehensive treatment modality for tumors with diverse biology and different progression to achieve maximum tumor control and minimize complications. However, for advanced cancer, the combination of these traditional modalities has not been effective in increasing survival time. This method is a combination of management and clinical experience of doctors, oncologists with specialized therapeutic weapons to be able to treat cancer based on the right standards according to the criteria. The regimen has been scientifically studied and evaluated as effective, appropriate to the stage and circumstances of the disease.Recently, with the emergence of the fourth therapy, immunotherapy, there are many positive points. It seems that immunotherapy has overcome most of the shortcomings of traditional therapies such as no serious side effects, no side effects, no complications, and reduced risk of recurrence.

Sự so sánh giữa sử dụng và không sử dụng liệu pháp miễn dịch.
2. Cancer immunotherapies
2.1. Monoclonal Antibody Therapy (Passive Immunotherapy)
Are drugs designed to bind to a specific target in the body. These monoclonal antibodies stimulate the immune system to produce cells that can destroy cancer cells. Another form of monoclonal antibody can mark cancer cells, making it easier for the immune system to locate and destroy cancer cells. These types of monoclonal antibodies can be considered as a targeted therapy.
There are many types of monoclonal antibodies and each type of antibody has different functions through many mechanisms leading to cell death. Some of the mechanisms include blocking the signaling pathways needed for cell growth, manipulating the immune system's response to toxins, preventing tumor growth, and so on. Monoclonal antibodies have been used. in the treatment of leukemia, breast cancer, bowel cancer, and head and neck cancer. These clinical trials are still underway in phase III and promise to bring many expected results for patients in the future.
2.2. Checkpoint Inhibitors
When cells are in a normal state, our body's immune system depends on "recognition points" or "immune breakpoints" to avoid over-activating the immune system. Tumor cells often take advantage of these markers to avoid detection by the body's immune system. CTLA-4 and PD-1 are markers that have been studied and are in clinical use as an anticancer therapy. CTLA-4 is commonly found on the surface of T cells and is often aberrantly upregulated in several major cancers. PD-1 has also been found to upregulate in some cancers, PD-1 inhibits T-cell function and, at the same time, indirectly enables tumors to escape immune control. Translate. Inhibiting “recognition points” or “release of barriers” is an effective therapy that can enhance T-cell responsiveness and help immune system cells attack cells. more effective tumor cells. There are now intensive phase III studies with specific drugs, some of which have been approved by the FDA for clinical use, with results showing promise for the future.2.3. Immune Regulatory Proteins (Cytokines)
Cytokines are proteins produced by the body's own cells, play an important role in the body's primary immune response and also have the ability to induce an immune response to cancer cells. There are two types of cytokines used in cancer treatment called Interferons and Interleukins.
The two most common cytokines are interleukin 2 (IL-2) and interferon α (IFN-α), which regulate the immune response. For example, IL-2 has many major effects on the immune system and acts as a normal growth factor for T cells. It then binds to receptors on the surface of T cells. This binding will regulate T cell growth, continue to produce cytokines, and activate many other types of immune cells. Results of treatment with high doses of IL-2 show that IL-2 can induce a complete immune response in 4% - 6% of patients with renal cell carcinoma and leukemia. This suggests that in this group of patients, IL-2 therapy is effective in the endogenous antitumor immune response.
2.4. Vaccines to treat cancer
Vaccines were previously understood as a therapy to prevent infection through antigen-antibody immunity, specifically, when a person is injected with a attenuated antigen of a pathogen to stimulate a specific immune response. host efficiency and robustness in subsequent infections . Today, in the field of oncology, the concept of a vaccine has a meaning and a therapeutic role, that is, increasing the immune system's response to cancer cells. Vaccines are derived from immune cells, designed, nurtured and trained outside the body and infused into the host so that they can modulate and increase the patient's immune system response to fight tumor antigens.
By activating the immune system, cancer treatment with vaccines can activate an anti-tumor response, which then attacks tumor cells and can improve patient survival time. It should be noted that vaccine therapy in cancer is different from the traditional preventive vaccines used in many infectious diseases. Simply put, the main purpose of vaccines in cancer therapy is not to prevent disease but to induce an active immune response against an existing cancer pathogen. Cancer therapy vaccines are given by injection or through a vein.

Bằng cách kích hoạt hệ miễn dịch, điều trị ung thư bằng vaccine có thể hoạt hóa một phản ứng kháng bướu, sau đó tấn công tế bào bướu và có thể cải thiện thời gian sống bệnh nhân.
3. Indications for treatment and response effectiveness of immunotherapy in cancer
3.1. Treatment strategies
Currently, immunotherapy is not as widely used in clinical practice as traditional therapies such as surgery, radiation therapy and chemotherapy. However, recently many immunotherapy drugs based on monoclonal antibodies (immune checkpoint inhibitors) have been approved for use in many different types of cancer such as blood cancer, liver cancer. , lung cancer, prostate cancer. There are many other cellular immunotherapies that are still in phase II and phase III clinical trials, and a few drugs that have been approved by the FDA for sale in the pharmaceutical market for cancer of the genitourinary system. blood, showed a clinically significant improvement.
For solid tumors, due to the diversity in tumor antigen expression, finding an effective vaccine is still a big challenge. Most of the trials are in phase II and phase III and have not yet been approved by FDA for clinical use
Immunotherapy drugs can be introduced into the body in many forms such as intravenous injection (medication given as an infusion) directly into a vein), orally (in pill or capsule form), topically (a cream applied to the skin used to treat early skin cancer), or injected directly into the bladder via a balloon urine . (immunotherapy is administered directly into the patient's bladder).
The course of immunotherapy depends on several factors:
The type of cancer the patient has and the stage of the disease. Immunotherapy drugs are used in the treatment. The body's response to immunosuppressive drugs. The treatment regimen must be strictly monitored on a daily, weekly and monthly basis. Some types of immunotherapy are indicated to be used according to the cycle of the regimen, besides between treatments, patients need to have appropriate rest periods for the body to have time to respond to the drug. regenerate and regenerate cells. Then, in order to evaluate the effectiveness of using immunotherapy in cancer treatment, the patient's disease progression and health status should be regularly and strictly monitored through physiological tests. disease, the body's resistance (expressed in the patient's perception and resistance during treatment). Patients will be checked for blood and tissue tests and some imaging tests such as CTscan, MRI, immunohistochemistry,...
3.2. Immunotherapy in multimodal therapy
Currently, immunotherapy in cancer is mainly reserved for advanced disease, so it is often used as the sole treatment. However, in response to tumor biodiversity, it is possible that one or more immunotherapies can be used to enhance tumor response.
In addition, there are recent clinical trials combining chemotherapy and immunotherapy to enhance tumor response and increase survival.
Furthermore, immunotherapy following tumor removal interventions has also been shown to reduce tumor recurrence time, which was previously clearly the role of adjuvant radiotherapy.
Several clinical trials are also currently directed towards the combination of radiation therapy and immunotherapy to enhance tumor response for advanced or recurrent head and neck cancer.
3.3. Some notes in cancer immunotherapy treatment
The advantages of immunotherapy are specificity and systemic action, few side effects and generally safety; However, the above immunotherapies still face some obstacles such as:
There is often a significant dependence between the total tumor cell mass and the body's immune response. The expression of oncogenes in the cells of a tumor is not uniform. Some tumor cells have the ability to produce factors that attenuate or suppress the immune response. In addition, possible side effects are an unavoidable part of cancer therapies. Side effects depend on the type of immunotherapy used and the body's response to each type of therapy. The most common side effect is a skin reaction at the injection site such as pain, swelling, redness, itching, or a rash. Patients may also experience flu symptoms such as fever, cold, dizziness, vomiting or headache, aches and pains, shortness of breath, irregular heartbeat and blood pressure, etc. In some cases, water edema, weight gain due to fluid retention, high heart rate, allergic inflammation, sinus congestion, diarrhea, and risk of other infections.
However, clinical trials have shown that the side effects of immunotherapy are negligible and safe for patients.

Các tác dụng phụ có thể xảy ra là một điều khó tránh khỏi ở các liệu pháp điều trị ung thư.
4. Conclusion
Immunotherapy in cancer treatment promises to bring many improvements in cancer survival, considered the fourth weapon of cancer treatment, after weapons such as surgery, chemotherapy and radiation.
Immunotherapy methods based on the suppression of immune checkpoints have been approved for clinical use by the FDA as proven effective through numerous phase III clinical trials.
Vaccine therapy for cancer by retransfusion of engineered, nurtured, and trained immune cells has been approved by the FDA for use in hematopoietic cancer.
For cancers of the solid tumor system, current vaccines are only tested in phases II and III and more research is needed to prove efficacy and allow clinical use
Immunotherapy is currently only for advanced cancer and is currently being tested in combination with other treatment modalities as an adjunct to surgery, chemotherapy, and radiation therapy.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.