This is an automatically translated article.
Article written by BS. Nong Ngoc Son - Doctor of Chemotherapy and Palliative Treatment, Oncology Center - Vinmec Central Park International General Hospital
Lung cancer is the most common type of cancer, in which non-small cell lung cancer accounts for 85 - 90%, the rest is small cell lung cancer (10 - 15%). Depending on the specific type of pathology, the doctor will have different treatment methods. In this article, we mainly deal with non-small cell lung cancer (NTPKTBN).
1. What are the stages of lung cancer?
To diagnose lung cancer, doctors will rely on the characteristics of disease symptoms (such as cough, chest pain, shortness of breath,...), laboratory results (such as chest X-ray, etc.) chest computed tomography, abdominal ultrasound,...).
In particular, doctors need to take a biopsy or poke a needle into the lymph nodes or tumor in the lung to get a sample of the tumor, then send it to the pathology laboratory.
Here, the pathologist will cut out the tumor samples and diagnose the disease based on the images under the microscope. Today, in addition to reading tumor images under a microscope, doctors also use molecular biology machines to identify lung cancers based on genetic mutations as well as the expression of other types of cancer. receptors located on cancer cells.
After confirming the diagnosis of lung cancer, doctors will evaluate the tumor size, tumor location, assess the status of lymph node metastasis as well as find the metastatic sites (if any) to evaluate disease stage. Non-small cell lung cancer has four stages from stage I to stage IV according to the classification system of the American Joint Committee on Cancer (AJCC) and the International Union for Cancer Prevention (UICC). .
Depending on the specific stage, doctors will advise the patient on appropriate treatment options such as surgery, radiation therapy or systemic treatments such as chemotherapy, targeted therapy, therapy, etc. immunity,...

2.What is immunotherapy?
Immunotherapy is the use of drugs to help the body's immune system fight cancer. Normally, the immune system will detect and destroy abnormal cells and will largely stop the overgrowth of many types of cancer.
However, cancer cells find a way to avoid the destruction of the immune system such as changes in genes and proteins to "avoid" immune cells. Immunotherapy helps the immune system recognize cancer cells and destroy them.
A number of immunotherapies are being studied and used in cancer treatment such as:
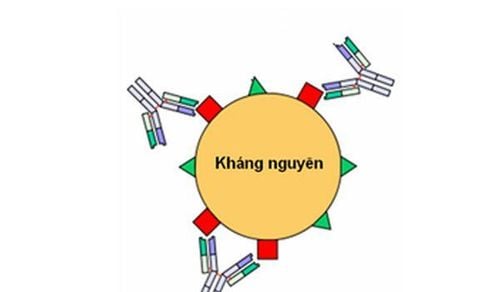
CAR-T cell therapy: Immune cells are removed from the patient's blood. After being processed to receive electricity specific to the type of cancer to be treated, these cells are transferred back into the patient's body. From there, these immune cells will help the body's immune system better fight tumor cells. Monoclonal antibody therapy: These are proteins of the immune system. Once attached to cancer cells, these monoclonal antibodies will help immune cells recognize and destroy cancer cells more easily. Therapeutic vaccines: Cancer cells contain substances called tumor-associated antigens. These antigens are inherently absent or very low on normal cells. Therapeutic vaccines help the immune system recognize and act on these antigens, helping to destroy cancer cells.
Immunomodulators: These are drugs that help regulate the body's immune system, increase the immune system's ability to fight tumors such as cytokines, BCG or immunomodulatory drugs such as thalidomide, lenalidomide, ... Cytokines are proteins made by blood cells (such as interferons, interleukins...) that help immune cells become more active and destroy tumors. Immune checkpoint inhibitors (ICIs): Immune checkpoint inhibitors are normal components of the immune system that control immune responses, not to the immune system. overactive. These drugs help block immune checkpoints, allowing immune cells to respond more strongly to cancer cells.
3. What are immune checkpoint inhibitors?
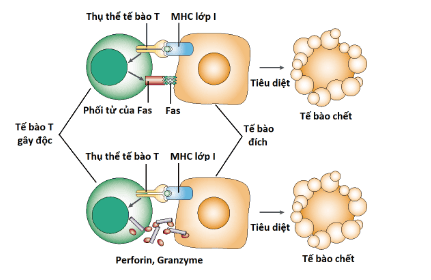
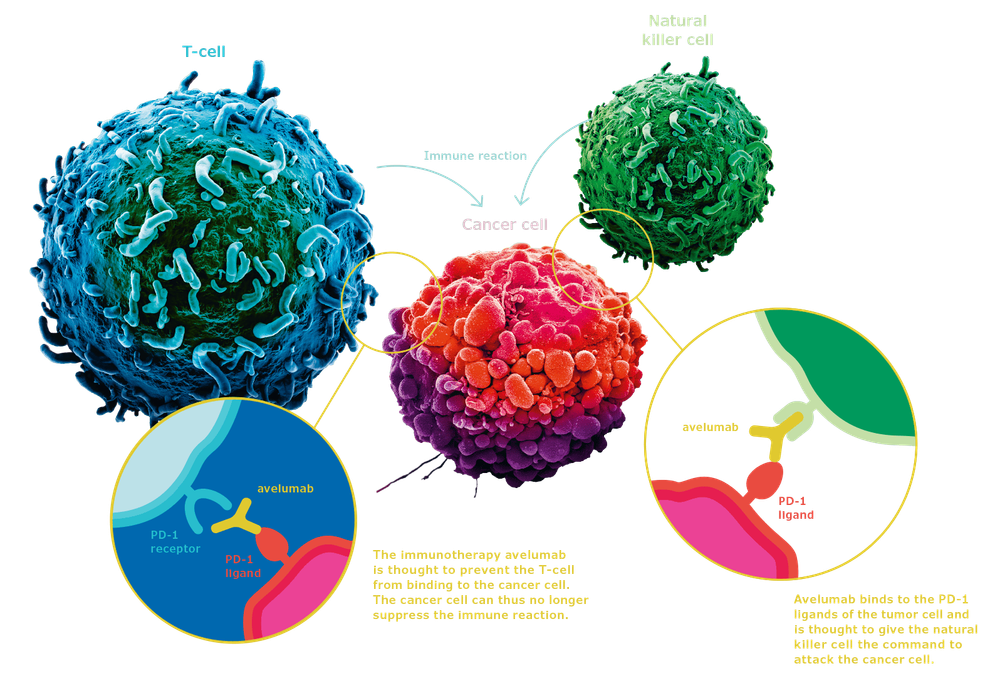
T cells are cells that play a very important role in the cellular immune response. There are receptors on the surface of T cells and tumor cells. Several receptors will act as co-activated immune checkpoints that promote T-cell activity against antigens (foreign cells).
Some receptors will play an inhibitory role, playing a role in protecting the body's normal, healthy cells. These promoters and inhibitors are normally in balance through complex regulation of the body. Cancer cells also rely on these immune checkpoints to escape the immune system.
Therefore, immune checkpoint inhibitors will target these immune checkpoints, helping T cells to better recognize tumor cells and destroy them.
A few immune checkpoints that are being studied a lot are PD-1/PD-L1, CTLA-4 ligand/CTLA-4. For the discovery of these immune checkpoints, professors James P. Allison and Tasuku Honjo were awarded the 2018 Nobel Prize in Biomedical Sciences.
4.Immune therapy in early lung cancer?
Immunotherapy is a newly introduced lung cancer treatment. In early stage (stage I or II) lung cancer, surgery is the mainstay of treatment. Depending on the specific situation, the doctor may recommend radiation therapy or chemotherapy.
In patients with stage III lung cancer, the choice of treatment methods such as surgery, chemotherapy or radiation therapy depends heavily on the size, location of the tumor, the status of lymph node metastasis as well as the possibility of Is surgery possible?
In many patients, a combination of chemotherapy and radiation therapy is considered the cornerstone of treatment if surgery is not possible. Despite a combination of treatments, the prognosis of patients with inoperable stage III lung cancer remains less favorable, with a 5-year survival time of only about 15%.
The PACIFIC study on more than 700 patients with inoperable stage III NSCLC who had previously received concurrent chemoradiotherapy but did not progress will be given the anti-PD-L1 antibody durvalumab. With a follow-up of about 25 months, use of durvalumab after concurrent chemoradiotherapy extended the survival time of patients compared with no treatment with durvalumab. This study helped the United States Drug and Drug Administration (FDA) approve the use of durvalumab in this stage of NSCLC.
5.Immune treatment in advanced metastatic stage?
In patients with advanced, metastatic non-small cell lung cancer without important gene mutations, immunotherapy has been shown to be beneficial in prolonging life.
Currently, factors that help select immunotherapy depend on the absence of important gene mutations, PD-L1 expression level, disease spread, and histology.
Specifically, according to the guidelines of the American Society of Clinical Oncology, patients with expression of PD-L1≥50% can receive anti-PD-1 antibody pembrolizumab, patients with expression of PD -L1<50% should be given chemotherapy in combination with pembrolizumab.
Based on the KEYNOTE-189 study reported at the American Association for Cancer Research annual meeting in Chicago in April 2020, after a median follow-up of approximately 10.5 months in 616 patients, patients who received chemotherapy in combination with pembrolizumab had a 51% reduced risk of death compared with those who received chemotherapy alone.
After 12 months, about 69.2% of the patients in the combination chemotherapy and pembrolizumab group were still alive, while in the chemotherapy alone group only 49.4% of the patients were alive. The time from treatment to progression was also longer in the pembrolizumab combination group (8.8 months) and nearly twice as long as in the chemotherapy group alone (4.9 months).
Overall, there was no significant increase in side effects in the pembrolizumab group, with the exception of a few patients (5.2% of patients) who had a greater decrease in renal function (renal failure) than in the group. only chemotherapy (0.5%).
Similarly, based on the IMpower 150 study of 1202 patients, a four-drug combination, including two chemotherapy agents, another new immunomodulator (atezolizumab) and a vascular antibiotic (bevacizumab) was also effective. results in improved survival time for patients.
In patients with high PD-L1 expression (≥50%), pembrolizumab or atezolizumab monotherapy also prolongs survival. Another option is a combination of nivolumab and ipilimumab that is equally effective.
In short, medicine today, with the great progress of science and technology, the future of lung cancer treatment will be brighter and brighter.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.