This is an automatically translated article.
The article is professionally consulted by Master, Doctor Nguyen Thi Ngoc - General Internal Medicine - Endocrinology - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital. Doctor has more than 10 years of studying, researching and working in the field of endocrinology.Water plays a very important role in participating in the structure of cells and organs, as well as maintaining normal activities in the body. When our body loses 10% of water, we are already in a pathological state, if we lose 20-25% of water, we can die. In the body, water is also the solvent for biological systems.
1. How is water distributed in the body?
On average, water accounts for about 70% of body weight and is unevenly distributed in different organs and organizations. The total amount of water in the body is not fixed but decreases with age.For babies, the total amount of water makes up about 75 - 80% of the body. From 1 year of age through middle age, total water intake makes up about 60% of body weight for men and 55% of body weight for women. After middle age, the total amount of water only accounts for about 50% of body weight.
Distribution of water in the body in 2 main compartments separated by cell membranes, that is:
Intracellular fluid compartment: accounted for 40% of body weight. Extracellular fluid compartment: Consists of 20% of body weight. In the extracellular fluid compartment, it is divided into 2 parts by the capillary membrane, which are:
Intercellular fluid (also known as interstitial fluid): accounts for 15% of body weight. Plasma: Consists of 5% of body weight.
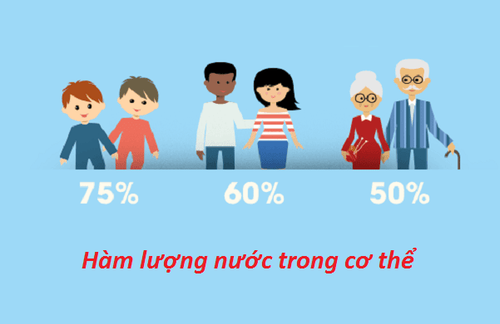
Tổng lượng nước trong cơ thể là không cố định mà giảm dần theo độ tuổi
2. Water balance in the body
Water balance in the body is the balance between the amount of water inside and the amount of water discharged. Every day, the amount of water in the body is provided through eating, drinking and endogenous water from metabolism.Water requirement for the body daily is about 2,000 - 2,500 ml, of which, oral is 1,000 - 1,200 ml, table sugar is 800 - 1,000 ml, and 200 - 300 ml from metabolism. The amount of water discharged includes 1,200 - 1,400 ml of urine, 400 - 500ml of respiratory tract, 300 - 500ml of evaporation through the skin and 100ml of feces. Water balance in the body also has an invisible loss of water that increases when having a fever is about 100 - 300 ml / 1 degree Celsius / day or 2 - 2.5 ml / kg / day for each degree above 37 degrees C, physiological sweat evaporation is about 500 ml/day, profuse sweating and high fever or dry environment with low humidity is 1,000 - 1,500 ml/day. Measured water loss is increased with diuretics such as hyperglycaemia and diuretics, bowel preparation, and adrenal disease.
Nhu cầu nước đối với cơ thể hằng ngày là khoảng 2.000 - 2.500 ml
3. Mechanism of exchange and metabolism of water in the body
Water balance is the process of exchange and metabolism of water in the body taking place in cell membranes and capillary membranes.3.1. Water metabolism across the cell membrane As for the cell membrane, because it is selectively permeable, the membrane allows only water and small-molecule organic substances to pass through (such as amino acids, glucose, etc.), and does not allowing large molecules to pass through (such as proteins, SO42-, PO43-, etc.).
Water exchange and metabolism in the cell membrane is actually the process of moving water between the inside and outside of the cell. Water is transported across the cell membrane due to the difference in osmotic pressure between the two compartments, the cavity with high osmotic pressure will move to that side.
3.2 Water metabolism across capillary membranes Water balance between plasma and intercellular fluids depends on the following factors:
Permeability of the vessel wall: The vessel wall is a barrier that allows all small molecules to pass through, except for molecules like proteins. The permeability of the vessel wall is influenced by factors such as: vasomotor nerve, the nutritional state of the capillary wall, etc. In diseases of hypoxia, vitamin deficiency, acidosis affecting endocrine and other diseases. chemical mediators, etc. can change the permeability of the vessel wall. Osmotic pressure and colloidal pressure in blood and interstitial fluid: The metabolism of water inside and outside the vessel wall is due to a balance between osmotic pressure, which tends to push water out, and colloidal pressure to draw water from the blood. outside in. In addition, there is some intercellular fluid that migrates in the lymphatic route. Neuro-humoral factors: Mainly due to ADH and aldosterone affecting the water balance in the body. ADH is secreted and stored in the posterior pituitary from the supraoptic nucleus and the subventricular nucleus in the suboptic area. The secretion of ADH is influenced by the osmotic pressure of the blood. When plasma osmotic pressure is increased, through receptors in the hypooptic area and some other organs such as liver, lung, pancreas, etc., it will increase ADH secretion. Thus, increasing water absorption has the effect of restoring plasma osmolality (eg, when drinking a lot of water, giving lots of fluids, etc.). Also through these osmotic receptors causes a decrease in ADH secretion, thereby reducing water reabsorption, this process has the effect of restoring plasma osmolarity. In addition to the osmotic receptors, there are also volumetric receptors that govern the secretion of ADH. Increased secretion of ADH is also seen in some cases such as pain, fear, muscle movement, morphine injection, bleeding, etc. ADH secretion is also done through a conditioned reflex mechanism - one of the roles of the brain. set. Aldosterone is the main hormone of the body's water balance mechanism, has the effect of reabsorbing Na and excreting K in the distal renal tubule. When the concentration of Na in the blood increases, the secretion of aldosterone decreases, which increases the excretion of Na. Conversely, when the concentration of Na in the blood decreases, aldosterone will increase secretion to increase Na reabsorption. Factors affecting aldosterone secretion: Na+ deficiency, K excess, decreased blood volume, trauma, emotion, ACTH, STH, post-pituitary hormone (increases secretion); Na excess, K deficiency, increased circulating blood volume, X-wire stimulation, right atrium dilatation, increased catecholamines, aldosterol antagonists (reducing secretion). In addition, renin also has a stimulating effect on aldosterol secretion. When blood pressure decreases, renin secretion increases leading to an increase in angiotensin II, which stimulates the adrenal cortex to increase aldosterol secretion. Conversely, when blood pressure is increased, renin secretion decreases leading to a decrease in aldosterol secretion. In some clinical syndromes, renin secretion is observed, associated with increased aldosterol secretion (blood loss, circulatory failure due to stasis, cirrhosis, etc.). Regulation of aldosterol also depends on volume receptors in the walls of the carotid artery, large arteries near the heart, atria, etc. Water distribution in the body helps the body maintain normal activities.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.













