This is an automatically translated article.
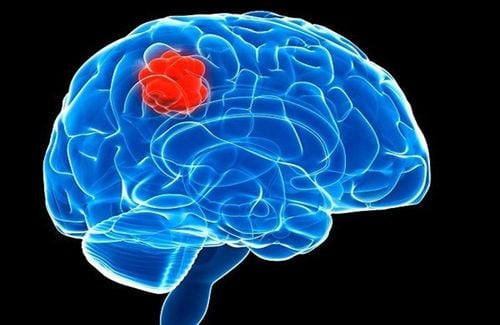
Meningiomas are the most common brain tumor - accounting for about 30% of all brain tumors - and most are treatable. In fact, the majority of these tumors are considered surgical intervention and most patients do not recur. Details about the treatment of meningiomas are presented in the following article.
1. Consider treatment decision
The treatment method indicated for each case of meningioma depends on many factors, including:
The size and location of the meningioma; The rate of growth or invasion of the tumor; The patient's age and overall health; The goal of long-term treatment.
2. Monitor disease progression
Immediate treatment is sometimes not necessary for many people with meningiomas, especially when it is only discovered by chance during cranial magnetic resonance imaging for another disease. In fact, a small meningioma that grows slowly and causes absolutely no signs or symptoms may not require treatment.
At this point, what needs to be done is to plan periodic follow-up by clinical examination as well as brain imaging. In this way, the doctor will evaluate whether the meningioma has progressed or not as well as its effects to guide intervention at the appropriate time.
3. Meningioma treatment options
Mục tiêu của phẫu thuật là để loại bỏ hoàn toàn khối u trên màng não
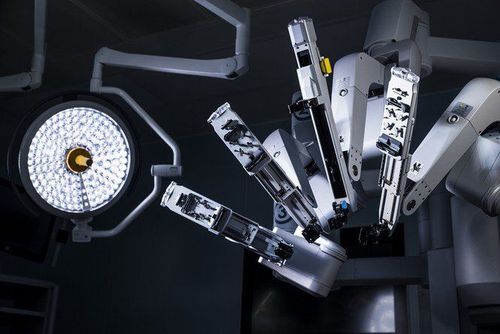
3.1 Surgical intervention Once your meningioma shows that it has caused symptoms or shows signs of growth, your doctor may recommend surgery.
The goal of surgery is to completely remove the tumor on the meninges . However, because meningiomas can be located near many other delicate structures in the brain or spinal cord, it is not possible to remove the entire tumor at once. In these cases, surgeons will consider removing as many meningiomas as possible.
Surgery can have risks, including infection and bleeding. The specific risks of surgery in each case will depend on the location of the meningioma. For example, surgery to remove a meningioma located around the optic nerve can lead to vision loss. Therefore, before making a decision, it is important to ask the surgeon about the specific risks that may occur.
After surgery, follow-up depends on a number of factors. If the tumor is no longer visible, no further treatment is usually needed. However, the patient will still need to have brain scans for periodic monitoring. If the tumor is determined to be benign in nature and only a few small fragments remain, your doctor may recommend periodic monitoring or possibly additional radiation therapy. Conversely, if the tumor is atypical or malignant in nature, you will need radiation therapy after surgical intervention.
3.2 Radiation Therapy If your meningioma cannot be completely removed with surgery, your doctor may recommend radiation therapy after surgery.
The goal of radiation therapy is to kill any remaining meningiomas and reduce the chance that the meningioma may recur in the future. This method uses a large machine that emits powerful beams of energy, targeting tumor cells.
Radiation therapy has now made great progress, with increasing radiation dose to meningiomas while reducing radiation to healthy tissue. Radiation therapy options for meningiomas include:
Radiosurgery: A type of radiation treatment that uses several powerful beams of radiation aimed at a precise point. Contrary to its name, this type of radiation therapy does not use a scalpel or cause any wound damage. Radiosurgery is usually done in an outpatient setting and takes only a few hours. This is an appropriate option for people with meningioma that cannot be removed with conventional surgery or meningioma that recur despite treatment; Fractional stereotactic radiotherapy: Deliver radiation in small fractions over time, such as a continuous daily treatment, for 30 days. This approach can be used for tumors that are too large or on tumors that may not be able to tolerate intense radiation therapy - such as tumors near the optic nerve; Intensity-modulated radiation therapy: A type of radiation therapy that uses computer software to adjust the intensity of radiation directed at the meninges. This modality can be used for meningiomas located near sensitive brain structures or those with complex anatomical features; Proton beam radiation: The use of radioactive protons to precisely target the tumor, reducing damage to surrounding tissue. 3.3 Use of chemotherapy Chemotherapy or drug therapy is rarely used at baseline to treat meningioma. In fact, this option can again be used in cases that do not respond to surgery and radiation therapy.
No single chemotherapy regimen has been shown to be superior and universally accepted for the treatment of meningiomas. Therefore, currently, scientists are still working on chemotherapy methods that target molecular targets.

Hóa trị liệu hay điều trị bằng thuốc hiếm khi được sử dụng tại thời điểm ban đầu để điều trị u màng não
3.4 Other Alternative Treatments Alternative treatments, although unable to completely cure meningiomas, have some evidence to support their effectiveness. In particular, it is undeniable that with additional support from the outside, patients will reduce the side effects of specific treatments. On the other hand, they also help the patient to stabilize mentally and deal with the stress of being diagnosed with a meningioma.
Alternative medicine therapies that have proven useful include:
Acupuncture; Hypnosis; Massage; Meditation; Music therapy; Relaxation exercises. In short, meningioma is the most common tumor in brain parenchyma and current treatment measures have also achieved certain effects. However, in each specific case, it is necessary to discuss with your doctor to have the most appropriate treatment option, both to completely solve the meningioma, and to ensure quality of life.
Vinmec International General Hospital currently has the professional conditions and technical means to treat meningiomas. Vinmec gathers a team of highly qualified and experienced neurologists; modern medical equipment, up to international standards; professional service quality, helping to improve the efficiency of disease diagnosis and treatment.
For detailed advice on meningiomas and treatment methods, please come directly to Vinmec health system or register online HERE.
References: mayoclinic.org
MORE:
Structure of meninges Brain tumors in children: Causes, symptoms, diagnosis and treatment Differentiating encephalitis and meningitis in children