This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Gastroesophageal reflux disease (GERD) is a common gastrointestinal (GI) disease with worldwide prevalence and high prevalence in Western countries.
1. Gastroesophageal reflux disease overview
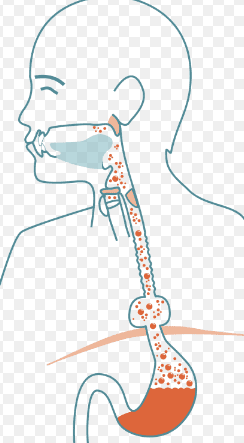
The 2006 Montreal Consensus defined gastroesophageal reflux disease as a condition that develops when the reflux of gastric contents causes bothersome symptoms and/or complications into the esophagus. Tissue damage associated with gastroesophageal reflux disease ranges from esophagitis to Barrett's esophagus and adenocarcinoma of the esophagus; The troubling symptoms of reflux can be esophageal (regurgitation, regurgitation) or extraesophageal. Gastroesophageal reflux disease can be further classified by the presence of an erosive stain on endoscopic examination (Erosive Reflux Disease [ERD] and Non-Erosive Reflux Disease [NERD]).
Extraesophageal manifestations associated with gastroesophageal reflux disease are frequent and represent a diagnostic and therapeutic challenge, possibly involving the lungs, upper respiratory tract, and mouth, presenting with asthma, laryngitis, chronic cough, tooth wear and non-cardiac chest pain
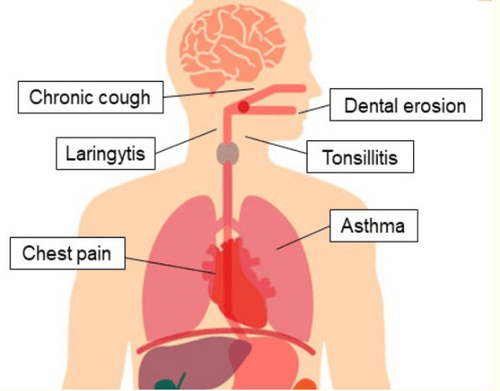
It is estimated that one-third of patients with GERD may have atypical extraesophageal or extraesophageal symptoms: noncardiac chest pain is the most common complaint (23, 1%), followed by pulmonary manifestations (bronchitis - 14.0%, asthma - 9.3%) and symptoms in the head and neck (hoarseness - 14.8%, visual sensations - 9.3%) demand - 7.0%) . In a prospective European study, the prevalence of extraesophageal symptoms was 32.8% in patients complaining of heartburn, with a higher prevalence in those with ERD (34, 9%) compared with those with NERD (30.5%). Chest pain (14.5%), chronic cough (13%), laryngeal disorders (10.4%) and asthma (4.8%) were the most common disorders associated with GERD. esophageal thickening.
2. Expression in the respiratory system
Several epidemiological studies have suggested an association between gastroesophageal reflux disease and respiratory symptoms, although a causal link has not been proven. Here, we discuss the most frequently reported pulmonary manifestations of gastroesophageal reflux disease: Chronic cough, asthma, and aspiration pneumonia.
2.1. Chronic Cough Cough is defined as chronic when it lasts more than 8 weeks; A much more persistent cough is defined as a chronic cough that is intractable. Common causes of chronic cough are side effects from commonly used medications (especially ACE inhibitors), tracheomalacia, chronic obstructive pulmonary disease (COPD), bronchiectasis. , asthma, obstructive sleep apnea, meningitis, and gastroesophageal reflux disease. In non-smoking, normal chest X-rays without ACE inhibitors, chronic cough was identified in 86% of cases as asthma, postnasal drip syndrome (PNDS), and Gastroesophageal reflux disease, although often multiple causes coexist.
Difficulty in diagnosing a cough due to reflux
When gastroesophageal reflux disease causes a cough, digestive symptoms can be absent up to 75% of the time, making the diagnosis more difficult. Furthermore, cough and gastroesophageal reflux disease are common and often coexisting diseases, but an association does not imply a causal relationship in all cases: Eastburn et al. flags in 25% of cases. The time relationship between reflux episodes and cough may help accurately resolve chronic cough with reflux, although diagnostic gold standards are lacking.
Patients with laryngeal or pulmonary manifestations of gastroesophageal reflux disease are usually seen first by an otolaryngologist, and only when a second presentation is present should they be referred to an otolaryngologist. receiving department of gastroenterology. In such typical situations, an upper gastrointestinal endoscopy is often indicated.
Role of gastroesophageal endoscopy
Normal endoscopy of the esophagus (gastroesophageal endoscopy) is a common finding in patients with cough due to gastroesophageal reflux disease; Only a few have esophagitis or Barrett's epithelium. Therefore, a normal esophagogastroduodenoscopy does not rule out the presence of gastroesophageal reflux disease or associated pulmonary abnormalities. Therefore, upper endoscopy should not be performed to diagnose asthma, chronic cough, or laryngitis associated with gastroesophageal reflux disease. Furthermore, the diagnosis of esophagitis did not confirm a relationship between gastroesophageal reflux disease and potential extraesophageal manifestations.
Treatment
Although there is little evidence to support this approach, PPIs are the most common treatment used in cases of suspected chronic cough due to gastroesophageal reflux disease. Several studies have shown improvement of chronic cough with this treatment; however, a recent randomized controlled trial (RCT) did not show a difference between PPIs and placebo. Explanation can be found in the small sample size included and in the types of quality of life (QoL) questionnaires used to address the usefulness of treatments.
Clinicians prescribing PPIs should consider their potential side effects, and maintenance treatment should be planned only when proven helpful.

2.2. Asthma Asthma is defined by the American Thoracic Society (ATS) as “a condition with a history of episodes of wheezing, coughing, or dyspnea and an increase in forced expiratory volume in one second (FEV1) by 20% from baseline after administration or reduction of bronchodilators. in FEV1 is 20% after bronchoalveolar transplantation with methacholine”.
Gastroesophageal reflux is suggested as a cause of asthma, as well as when clinically silent, and an effective reflux treatment may improve asthma control.
Significant association between asthma and gastroesophageal reflux disease
A significant association between asthma and GERD has been demonstrated in epidemiological studies: up to 50 % of asthmatic patients with associated gastroesophageal reflux disease. However, the prevalence of asthma in patients with gastroesophageal reflux disease is uncertain.
Treatment of reflux asthma Lifestyle changes, such as elevating the head of the bed, stopping smoking, and dietary changes (reduced fat, chocolate, alcohol, citrus, tomatoes, coffee and drinking tea, avoiding large meals, and eating three hours before bedtime) are recommended to improve reflux control and may help improve bronchial symptoms, although there are no RCTs to confirm this hypothesis .
Practical recommendations in patients with GERD-associated asthma (with or without esophageal symptoms) include initial empiric testing of PPIs once or twice daily days for 2-3 months. In patients who respond to therapy, PPIs should be tapered to the minimum dose necessary to control symptoms. In unresponsive cases, testing reflux with pH testing or impedance-pH monitoring can rule out pathological reflux.
In some studies, antireflux surgery has shown some beneficial effects on GERD-associated asthma: decreased disease control scores and asthma medication consumption asthma is reduced. However, a lack of consistent evidence encourages routine use of this method and further investigation is warranted.
2.3. Laryngitis Laryngo-pharyngeal reflux (LPR) is defined by the 2002 consensus of the American Academy of Otolaryngology Surgeons as a disorder of the backward flow of gastric contents into the larynx and pharynx. . This is a common extraesophageal presentation associated with gastroesophageal reflux disease: Up to 10–15% of all visits to ENT clinics are due to manifestations of laryngeal reflux- oropharyngeal
Gastroesophageal reflux disease can cause many symptoms in the larynx, such as hoarseness, pain or burning in the throat, pain when swallowing, feeling of lump in the throat, cough, throat clearing repetitive, sputum, difficulty swallowing and voice fatigue. These complaints are not specific to gastroesophageal reflux disease and laryngopharyngeal reflux disease, and they may also be caused by allergens, smoke, and various irritants.
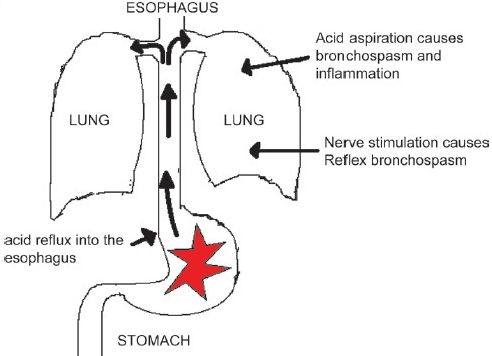
The laryngeal manifestation of gastroesophageal reflux disease can be explained by direct damage caused by acid-peptide contact in the larynx through esophageal-pharyngeal reflux (micro-aspiration theory). ), or by indirect acidification of the distal esophagus via an intermediate reflex (esophagobronchial reflex theory). Both mechanisms lead to chronic clearing of the throat and cough, causing mucosal damage and typical signs and symptoms.
Laryngeal mucosa is more susceptible to damage than esophageal mucosa: Acid reflux, containing acid and pepsin, and bile reflux cause inflammatory lesions and precancerous lesions of the larynx. However, the inability to clear saliva leads to more severe damage than that of the esophagus.
Diagnosis Laryngoscopy revealed reflux-mediated disease as congestion, edema, lymphatic hyperplasia in the posterior wall of the larynx, ulceration, stenosis of the lower glottis or posterior glottis, vocal cord polyps, granulomas, leukemia and cancer. Although common in reflux laryngitis, most of them are nonspecific. Edema and congestion, commonly used to define reflux laryngitis, lack specificity and are highly operator-dependent parameters. In fact, signs of laryngeal irritation were present in more than 80% of healthy controls. Allergies, smoking, and voice abuse are common causes of laryngeal irritation and cause similar alterations of laryngopharyngeal reflux.
Treatment of GERD-induced laryngitis Empiric PPI therapy over a period of one or two months is a reasonable initial approach in patients with no warning symptoms and a high suspicion of associated laryngeal disease. Reflux. If symptoms improve, therapy can be continued for up to 6 months to allow healing of laryngeal tissue, after which the dose should be tapered to minimal acid suppression, resulting in a sustained response. In patients who do not respond to PPIs, impedance or pH monitoring may be used to rule out reflux as the cause of laryngeal complaints.
Among the non-pharmacological treatments for laryngopharyngeal reflux, dietary changes appear to be effective: Patients following a low-fat, high-protein, and alkaline diet have a resolution rate symptoms are higher. However, a recent systematic review concluded that there is insufficient evidence to recommend dietary modification for laryngopharyngeal reflux.
Currently, Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for digestive diseases, diseases that cause chronic diarrhea, Crohn's disease, gastric mucosa Esophageal ectopic... Along with that, at Vinmec Hospital, screening for gastric cancer and gastric polyps is done through gastroscopy with Olympus CV 190 endoscope, with NBI (Narrow) function. Banding Imaging - endoscopy with narrow light frequency) results in clearer images of mucosal pathology than conventional endoscopy, detecting ulcerative colitis lesions, digestive cancer lesions Early stage...
Vinmec Hospital with modern facilities and equipment and a team of experienced experts, always dedicated to medical examination and treatment, customers can rest assured with internal services. gastroscopy and esophagoscopy at Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References 1. Marilena Durazzo,1,2,* Giulia Lupi, Extra-Esophageal Presentation of Gastroesophageal Reflux Disease: 2020 Update, J Clin Med. 2020 Aug; 9(8): 2559.Vakil N., Van Zanten S.V., Kahrilas P., Dent J., Jones R., Global Consensus Group The Montreal definition and classification of gastroesophageal reflux disease: A global evidence-based consensus. Am. J. Gastroenterol. 2006;101:1900-1920. doi: 10.1111/j.1572-0241.2006.00630.x. [PubMed] [CrossRef] [Google Scholar]