This is an automatically translated article.
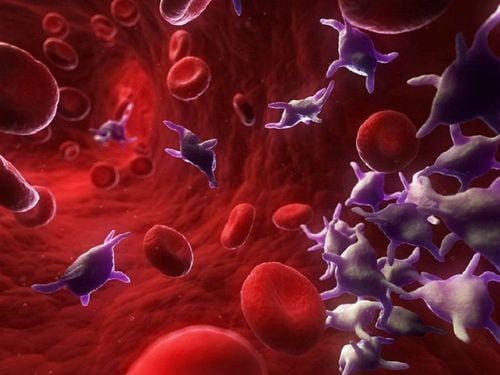
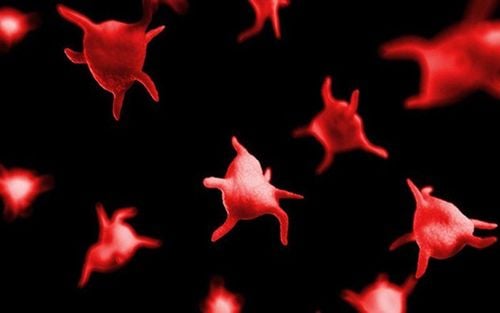
Idiopathic thrombocytopenia hemorrhagic disease is a type of autoimmune disease in humans, caused by a decrease in platelets in the body and affects the body's hemostasis and clotting function when there is a wound or slight impact. The disease is common in all ages, but the most common is thrombocytopenia in newborns and often leaves very serious complications.
1. Idiopathic thrombocytopenic purpura
Idiopathic thrombocytopenic purpura or immune thrombocytopenic purpura is one of the most common immunological diseases today, appearing in both adults and children, in which thrombocytopenic purpura in neonates. accounted for the highest percentage. This pathology is caused by the breakdown of platelets present in the peripheral blood on the endothelial reticular system with antiplatelet autoantibodies. Clinically idiopathic thrombocytopenic purpura can be acute, chronic, or relapsing. For the acute disease, the peripheral blood platelet count will return to normal value after 6 months and do not recur, while for the chronic form, the patient may relapse many times after. during treatment.
Xuất huyết giảm tiểu cầu xảy ra nhiều nhất ở trẻ sơ sinh
In idiopathic thrombocytopenic purpura, there will be the presence of antibodies against platelet antigens, which are IgG antibodies that can conjugate IgM and IgA. The mechanism of destruction of platelet cells is because antibodies attached to the surface of platelets in the peripheral blood will be destroyed by macrophages present in the endothelial reticular system, the most common site of destruction is the spleen. In addition, it can also destroy platelets in the liver or bone marrow. Some typical symptoms of idiopathic thrombocytopenic purpura include:
Subcutaneous haemorrhage: The patient has raised hemorrhagic organizations under the skin, which may be in the form of dots, nodules, patches or clusters. The color is very diverse, can be red, green, yellow or purple, bleeding gums, nose bleeds, vomiting blood or black stools, menorrhagia, hematuria... Anemia: Because the patient has Hemorrhagic, so if the bleeding is severe, it can lead to anemia. Liver, spleen as well as peripheral lymph nodes have no signs of abnormal enlargement. For subclinical, patients with idiopathic thrombocytopenic purpura will have some of the following signs:
Platelet count less than 100G/L Red blood cells, hemoglobin, normal white blood cells Red blood cells and hemoglobin have May be reduced in patients with severe bleeding With myelogram, myeloid cell density may be increased or within normal limits, platelet count within normal or increased range, red blood cells and white blood cells normal, no malignant cells present. Bleeding time longer than normal The clot may not contract or contract weak PT, APTT, TT, Fibrinogen normal Anti-GPIIb-IIIa antibody positive

Bệnh nhân bị bệnh xuất huyết dưới da
2. Is thrombocytopenia hemorrhagic disease hereditary?
In addition to the causes of thrombocytopenia bleeding, such as viruses, antiplatelet drugs, cancers, especially diphtheria, chemotherapy, aplastic anemia, splenomegaly, pregnant women pregnancy or idiopathic thrombocytopenic purpura, thrombocytopenic purpura can also be caused by genetic factors.
More specifically, a number of studies around the world have suggested that genetic diseases such as Bernard Soulier as well as MYH9 are related to thrombocytopenic purpura secondary to genetic mutations in these diseases. Therefore, in clinical practice, when finding the cause of thrombocytopenic purpura, besides clinical examination, examine typical signs such as subcutaneous bleeding, anemia, consider laboratory tests such as: the number of platelets, red blood cells, etc., it is extremely important to exploit the patient's family history, potentially heritable diseases that family members as well as the patient have had. , ensuring the correct diagnosis of the cause for the most effective treatment.
3. Hemorrhagic complications of immune thrombocytopenia?
Idiopathic thrombocytopenic purpura is an extremely dangerous disease that can threaten the life of the patient. This problem is explained as follows, when the platelet count in the peripheral blood of a person drops too much below the allowable level, hemorrhagic complications will appear, even if the patient only needs a very slight collision, the condition will be severe. Bleeding was very likely.
Xuất huyết giảm tiểu cầu có thể gây nguy hiểm đến tính mạng người bệnh
Thrombocytopenic purpura in children, especially thrombocytopenic purpura in neonates, can resolve on its own without any treatment. The time it takes for patients to recover is about 3 months, but there are also some cases of thrombocytopenia. There are a few cases that do not heal completely, but turn into a chronic form of this disease. As for idiopathic thrombocytopenic purpura in adults, it requires treatment, has a high probability of becoming chronic and often recurs.
Idiopathic thrombocytopenic purpura is a disease related to the immune system, mainly caused by autoantibodies against peripheral blood platelet cells. For neonatal thrombocytopenic purpura, the course is simpler and most likely to self-recover, while in adults, the disease can progress to a chronic stage and require different treatment methods. .
For detailed advice on immune thrombocytopenic purpura, please come directly to Vinmec health system or register online HERE.
SEE MORE
Diagnosis and treatment of Immune thrombocytopenic purpura Symptoms and complications of Immune thrombocytopenia Hemorrhagic fever How do platelets decrease?