This is an automatically translated article.
Helper T cells (or CD4+ T cells) were discovered in 1966 by a team of researchers at the University of Colorado in the US. These are cells that play a vital role in the immune system response. of body. After being differentiated and matured, helper T cells migrate to the lymph nodes, peripheral tissues, or peripheral circulation of the body.1. The role of helper T cells in the adaptive immune system
Helper T cells are considered to be the most important cells in the adaptive immune system, as they are essential for most adaptive immune responses in the body. These cells not only help activate B cells to secrete antibodies and macrophages to destroy the bacteria that are consumed into the body, but also help activate cytotoxic T cells to destroy the infected target cells. infection. In patients with AIDS, without helper T cells, their bodies would not be able to protect themselves even against many harmless bacteria.However, the helper T cell itself can only function when activated to become an effect cell. They are activated on the surface of antigen-presenting cells (APCs), which are cells that mature during the innate immune response to infection.
Tế bào T hỗ trợ là những tế bào quan trọng của hệ miễn dịch
2. Signals that help activate helper T cells
To help activate cytotoxic T cells or helper T cells to proliferate and differentiate into effective cells, an antigen presenting cell will provide the following 2 types of signals, including:Signal 1 : Provided by a foreign peptide bound to the MHC protein on the surface of the presenting cell. This peptide-MHC complex signals through the T cell receptor and its binding proteins. Signal 2: Provided by stimulating proteins, especially B7 proteins (including CD80 and CD86). Normally, the B7 protein will be recognized by the CD28 co-receptor protein on the surface of T cells. Expression of this protein on antigen-presenting cells (APCs) is induced by the pathogen during the response. innate immunity to infection. The efficacious T cell is reactivated to promote the expression of the B7 protein on antigen-presenting cells and induces a positive feedback loop that amplifies the T cell response. is thought to amplify the intracellular signal transduction triggered by signal 1. If a T cell receives signal 1 but does not receive signal 2, it may undergo apoptosis (apoptotic cell death). program) or changed so that it can no longer be activated, even if it subsequently receives both signals. This is one mechanism by which T cells can become tolerant to self-antigens.
Two signals activate helper T cells, including:
Mature antigen-presenting cells provide both signals 1 and 2, which in turn activate T cells. Immature antigen-presenting cells signal 1 but not signal 2, which kills or inactivates the T cell. On the other hand, the T cell receptor does not act on its own to transmit signal 1 into the cell. Instead, it binds to an immutable transmembrane protein complex, called CD3, which converts the binding of the peptide-MHC complex into intracellular signals. In addition, the CD4 and CD8 co-receptors play an integral role in signal transduction.
The combined actions of both signaling 1 and 2 help stimulate T cells to proliferate and initiate differentiation into effector cells by a strange indirect mechanism. In culture, they induce T cells to stimulate their own proliferation and differentiation by causing the cells to secrete IL-2 (a Cytokine) and simultaneously synthesize cell surface receptors that have High affinity binds it.
Binding of IL-2 to IL-2 receptors activates intracellular signaling pathways, opening genes that help T cells to proliferate and differentiate into effector cells. This mechanism also ensures that T cells differentiate into effector cells only when large numbers of them react with antigens simultaneously at the same site, e.g. in lymphocytes during infection. . Only then will IL-2 reach a high enough level to be effective.
Bản thân tế bào T hỗ trợ chỉ có khả năng hoạt động khi được kích hoạt
3. Subclasses of helper T cells help determine the nature of the adaptive immune response
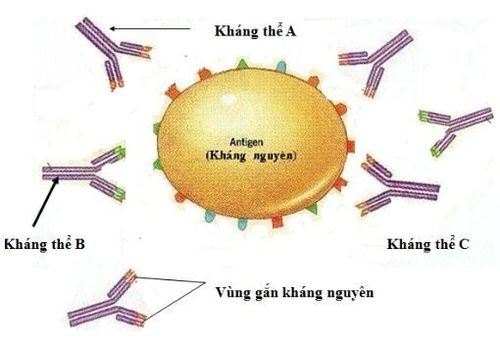
When an antigen-presenting cell (APC) activates "intact" helper T cells in peripheral lymphoid tissue, the T cells can differentiate into effective helper cells for T cells or T cells. 2.Two functionally distinct subclasses of helper T cells can be identified by the cytokines they secrete. If the cell differentiates into a T-cell, it secretes interferon-γ (IFN-γ) and tumor necrosis factor-α (TNF-α), and activates macrophages to destroy pathogens. bacteria in phagocytosis. Besides, it will also activate cytotoxic T cells to destroy disease-carrying cells. Although in this way T cells primarily defend the body against intracellular pathogens, they can also stimulate B cells to secrete specific subclasses of IgG antibodies that help cover foreign bacteria enter and activate complement.
In contrast, if an “intact” helper T cell differentiates into a T H 2 cell, it will secrete interleukins 4, 5, 10 and 13 (IL-4, IL-5, IL-10 and IL-). 13), which mainly protects the body against extracellular pathogens. On the other hand, T cells 2 can stimulate B cells to produce most classes of antibodies, including IgE and several subclasses of mast cell-binding IgG antibodies, basophils, and eosinophils acid . These cells release local mediators that cause conditions such as coughing, sneezing or diarrhea, which help expel extracellular bacteria as well as larger parasites from the epithelial surface. of body.
Thus, the differentiation of "intact" helper T cells into effective TH 1 or TH 2 cells has a significant effect on the type of adaptive immune response that will be mounted against the pathogen (for whether it will be mediated by macrophage activation or antibody production).
Specific cytokines present during helper T cell activation have a great influence on the production of effector cells. Bacteria at the site of infection not only induce dendritic cells to produce B7 co-stimulating proteins, but they also produce cytokines. The dendritic cells then migrate to a peripheral lymphoid organ and activate “intact” helper T cells to differentiate into effector TH1 or TH2 cells, depending on the cytokines produced by dendritic cells.
In people infected with the bacteria that cause leprosy, they multiply mainly in macrophages and cause one of two forms of the disease, depending mainly on the genetic makeup of the infected individual. For some patients may have tuberous leprosy. The H1 T cells will grow and stimulate the infected macrophages to destroy the bacteria. This has led to a local inflammatory response, causing skin and nerve damage. In contrast, some other cases may be infected with leprosy. H2 T cells grow and stimulate antibody production. Because these antibodies cannot penetrate the plasma membrane to attack intracellular bacteria, the bacteria multiply uncontrollably and can be fatal to the patient.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: ncbi.nlm.nih.gov