This is an automatically translated article.
Posted by Specialist I Vo Khac Khoi Nguyen - Orthopedic Trauma Doctor - General Surgery Department - Vinmec Central Park International General Hospital.
Fractures are a serious problem in both type 1 and type 2 diabetes. Healing of broken bones in diabetics is more difficult due to bone microstructural changes that reduce bone quality. Diabetes increases the risk of fractures in both men and women.
In people with type 1 diabetes, the risk of fracture is increased and fracture healing becomes more difficult due to decreased bone density. This is associated with decreased bone formation due to insulin and insulin-like growth factor-1 (IGF-1) deficiency. People with type 2 diabetes often have normal or high bone mineral density but are still at risk for fractures and delayed bone healing due to reduced bone strength.
1. Bone healing in normal people
2. Impact of diabetes on fracture healing
The healing of fractures in patients with diabetes takes 87% longer than in the general population and is 3.4 times more likely to have complications. These complications include delayed bone healing, failure to heal, or the creation of a prosthetic joint. Human clinical studies have shown that diabetes slows fracture healing. This is characterized by decreased adhesion and mineralization of the broken bone. It is hypoinsulinemia, increased insulin resistance, hyperglycemia, and oxidative stress that are the mechanisms that influence fracture healing in diabetics. These mechanisms may reduce osteoblast differentiation (osteocyte precursors), increase osteoclast activity, and lead to impeding fracture healing in patients with diabetes.

However, there is a significant difference in the skeletal effects between the two types of diabetes. Accordingly, type 1 diabetes has a great influence on bone mass and type 2 diabetes affects bone quality. This reduces the ability to heal broken bones.
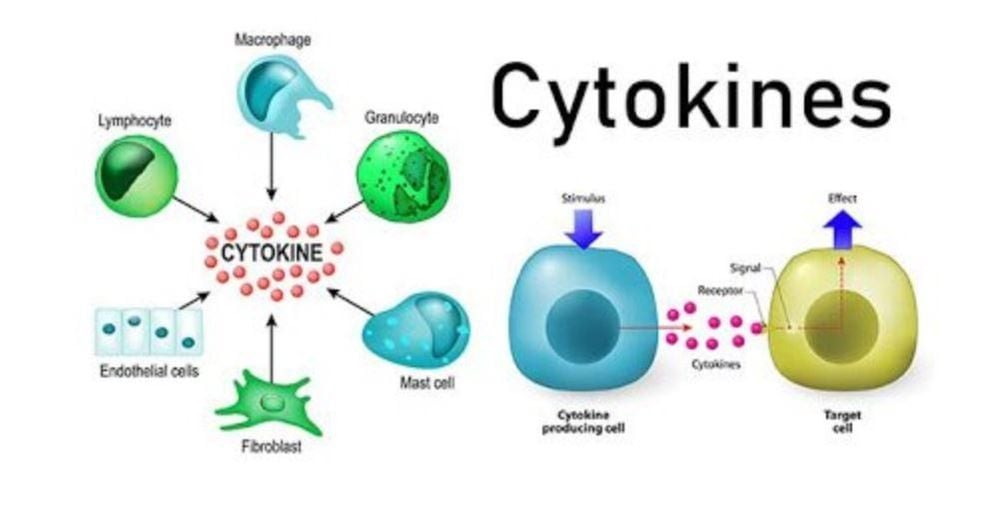
Diabetes leads to hyperglycemia, intensifying and perpetuating inflammation. These disorders as well as insulin resistance slow down bone healing. Especially when the fracture is accompanied by wound (open fracture), infection or other accompanying diseases that disturb the homeostasis in the body. All of these conditions are detrimental to fracture healing.
In addition, complications of diabetes affect the vascular system in the form of macrovascular and microvascular disease. This is easily seen by prolonging the wound healing process in diabetics. Both types of diabetes lead to atherosclerosis, which contributes to impaired wound healing and fractures.
3. Insulin and bone healing

Insulin acts directly on osteoblasts through the mechanism of promoting cell proliferation, reducing cell death, increasing glucose absorption, increasing collagen synthesis. In contrast, osteoclast activity is impaired under the influence of insulin. Insulin treatment helps restore fracture healing. Fracture is a surgical emergency. In that situation, it is more necessary to stabilize blood sugar with insulin than with oral hypoglycemic tablets.
However, insulin also treats hyperglycemia, so it is not clear whether the positive results are due to the direct effect of insulin on bone cells, the indirect effects of stabilizing blood sugar, or both. Experiments were performed to study the effect of insulin administration at the fracture site on fracture healing. The injection of insulin at the fracture site in diabetic animals has been shown to improve fracture healing. In a non-diabetic rat model, insulin at the fracture site accelerated fracture healing but did not alter the overall outcome. The use of topical insulin strengthens blood vessels and increases mineralization and mechanical strength at the fracture site.
In short, diabetes slows down the healing of broken bones. This condition can be made worse by poor blood sugar control, wounds, and infection of the fracture site. Patients should be fully aware of these issues. Treatment of osteoporosis prevention, prevention of falls is still the best measure to avoid fracture complications in people with diabetes.
Vinmec International General Hospital always deploys a screening package for diabetes and dyslipidemia to help detect pre-diabetes early, accurately classify diabetes type, develop a nutritional regimen, according to the guidelines. Monitor to reduce the risk and complications caused by diabetes.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
SEE MORE
Diagnostic criteria for diabetes and pre-diabetes What are the complications of diabetes? How does diabetes cause osteoporosis?