This is an automatically translated article.
Antibiotics do not help many lower respiratory infections caused by viruses. While acute bronchitis usually does not require antibiotic treatment. Antibiotics for lower respiratory tract infections are mainly used for patients with acute exacerbations of chronic bronchitis or pneumonia. Accordingly, the indication of the drug for the treatment of bacterial lower respiratory tract infections is selected by considering the age of the patient, the severity of the disease, and the presence of the underlying disease.
1. Antibiotic therapy for bacterial pneumonia
The goals of using antibiotics for lower respiratory tract infections for bacterial pneumonia are to eliminate infection, reduce re-infection rates and prevent complications, and improve outcomes.
Treatment of pneumonia depends largely on the empiric use of antibiotic regimens against potential pathogens determined by the context in which the infection occurs and potential exposure to multi-organisms. resistant and more virulent pathogens (eg, community-acquired or hospital-acquired pneumonia, hospital-acquired pneumonia, ventilator-associated pneumonia). Accordingly, initial empiric drug selection for lower respiratory tract infections for hospitalized patients should be broad and include potentially pathogenic organisms based on laboratory data as well as clinical response. .
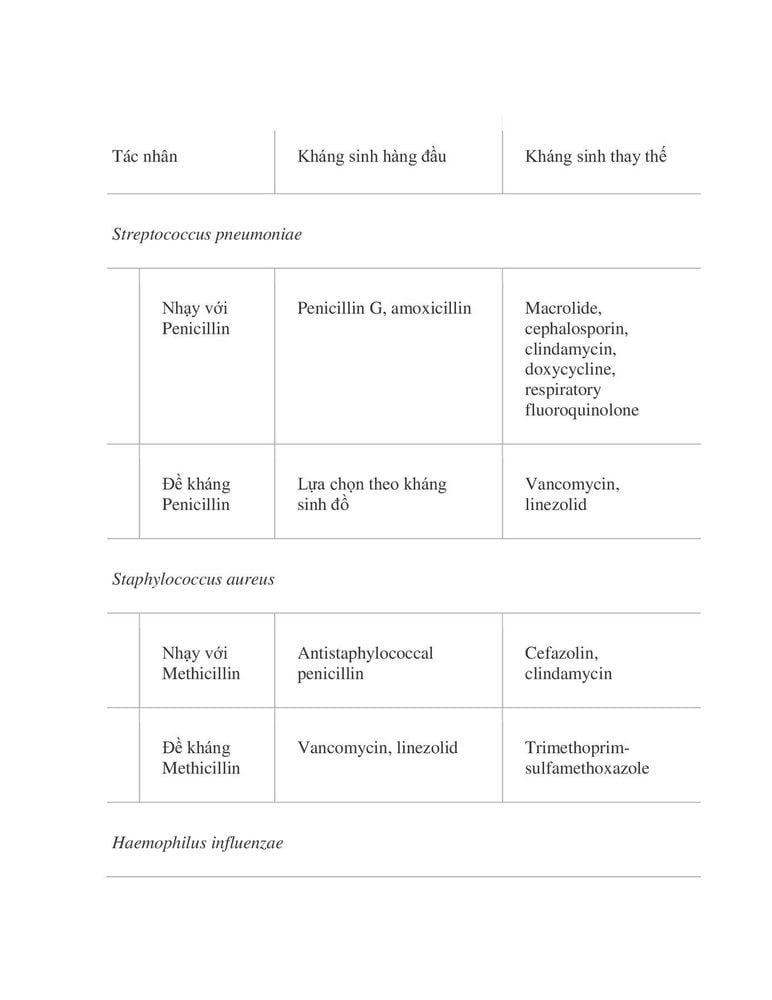
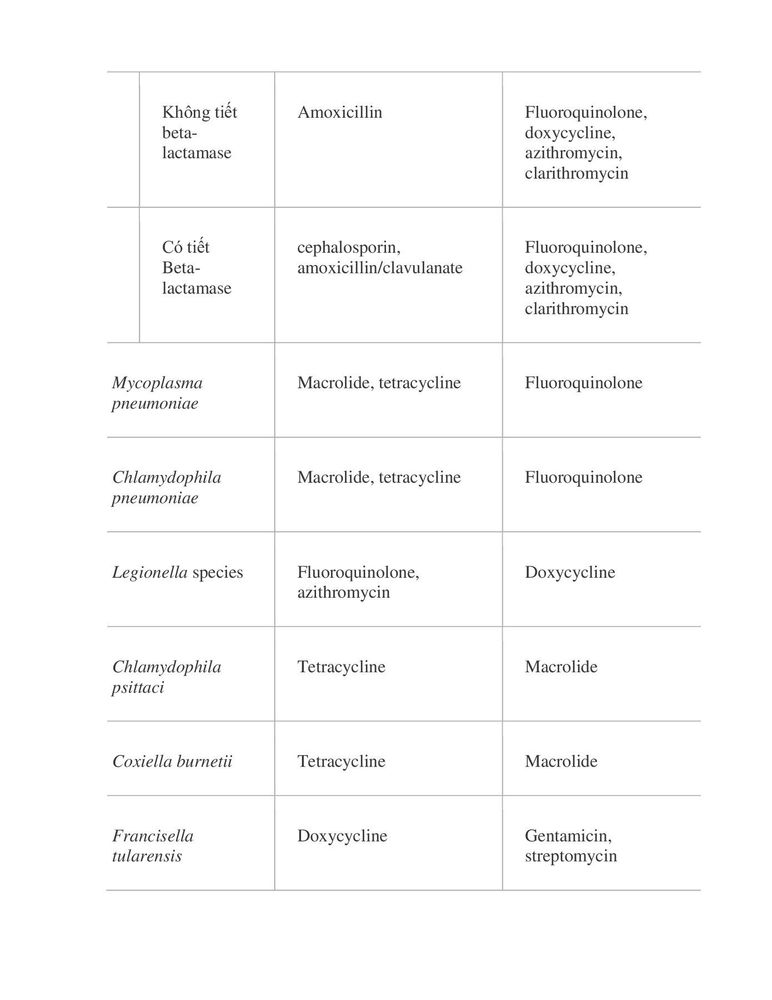
The possibility of Legionella infection should always be considered when evaluating community-acquired pneumonia, as delayed treatment significantly increases mortality. The most common pathogen is S pneumoniae, regardless of host or habitat. Empiric antibiotic therapy must be selected with this organism in mind.
Prevalence and resistance patterns of multidrug-resistant organisms vary between facilities and even between resuscitation units within the same facility. Therefore, the appropriate initial antibiotic class for lower respiratory tract infections for hospital-acquired or ventilator-associated pneumonia can vary markedly by hospital location. The practice of prescribing antibiotics is not necessarily based on national guidelines but on microbiological samples of multidrug-resistant organisms in each health care facility.
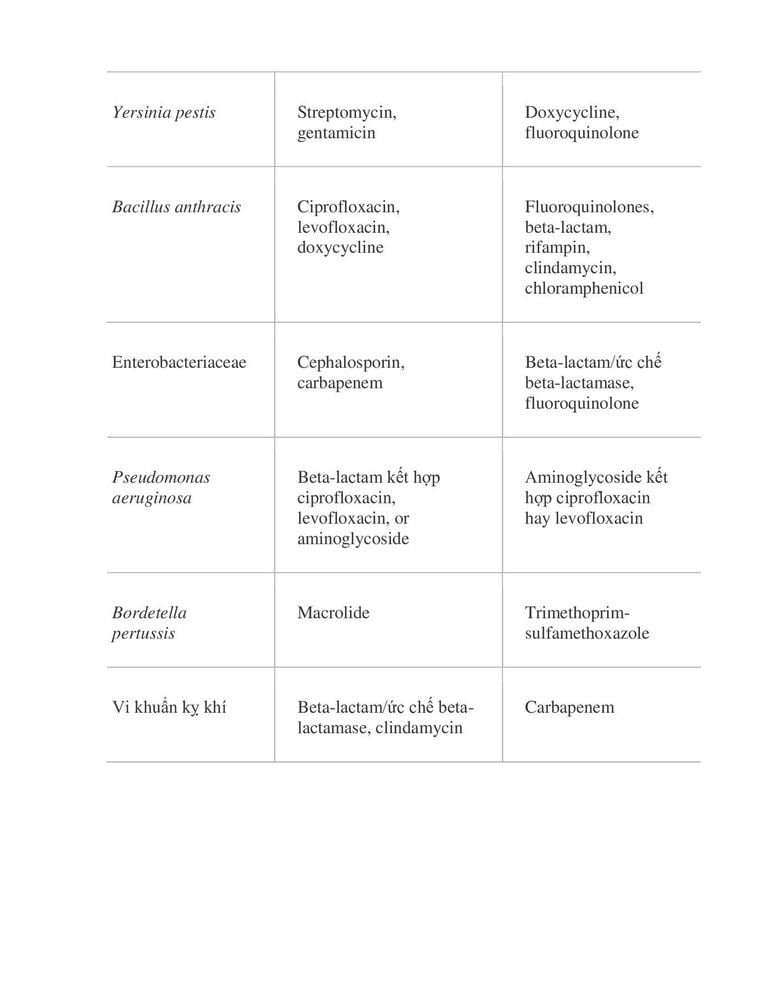
Accordingly, groups of antibiotics to treat lower respiratory tract infections for inpatients are as follows:
2. Empiric antibiotic therapy for outpatients
Outpatient drugs for lower respiratory tract infections should be selected based on the presence of patient risk factors, including recent antibiotic exposure, comorbidities, and trends in resistance. topical antibiotics.
In previously healthy patients not exposed to antibiotics within 90 days, use macrolides or doxycycline.
In patients with comorbidities such as chronic heart, lung, liver or kidney disease, diabetes mellitus, alcoholism, malignancy, immunosuppression (drug-induced or disease-induced) or drug use antibiotics within the last 90 days, use an inhaled fluoroquinolone or a beta-lactam plus a macrolide.
If the patient has been exposed to antibiotics within the previous 90 days for systemic treatment of any type of infection, an alternative agent from another class should be selected for the treatment of the current illness.
3. Empiric antibiotic therapy for inpatients
Inpatient treatment with drugs to treat lower respiratory tract infections in general, and pneumonia in particular, should be done within four hours of admission.
For patients not admitted to the intensive care unit, choose one of the lower respiratory tract infections intravenously or intramuscularly, including: Beta-lactam plus macrolide, Beta- lactam with doxycycline or antipneumococcal quinolone monotherapy.
If the patient is under 65 years of age and has no risk factors for resistant organisms, use macrolide monotherapy.
For patients with indications for admission to the intensive care unit, choose one of the following: Beta-lactam plus macrolide or Beta-lactam plus anti-pneumococcal quinolone.
If the patient has a documented beta-lactam allergy, administer antipneumococcal quinolones with aztreonam.
For patients at high risk for Pseudomonas infection, including patients entering and not entering the intensive care unit, choose from one of the following: Beta-lactam plus quinolone or beta-lactam plus quinolone antagonist aminoglycoside plus antipneumococcal macrolide or quinolone.
4. Empiric treatment of patients with aspiration pneumonia
Patients with severe periodontal disease, thick sputum, or a history of alcoholism with suspected aspiration lower respiratory tract infections may be at increased risk for anaerobic infections. One of the following antibiotic regimens is suggested for patients with aspiration pneumonia:
Piperacillin-tazobactam; Imipenem; Clindamycin or metronidazole plus inhalation fluoroquinolone plus ceftriaxone.
5. Empiric antibiotic therapy methicillin-resistant Staphylococcus aureus
For patients with suspected infection with methicillin-resistant S aureus (MRSA), vancomycin or linezolid, may be added to the antibiotic regimen until the identity of the organism and susceptibility to the antibiotic have been established. , at which point the medication can be adjusted accordingly.
Other classes of lower respiratory tract antibiotics that may be considered against MRSA include clindamycin, trimethoprim-sulfamethoxazole, gentamicin, ciprofloxacin, and rifampin.
In summary, an important consideration in the management of patients with lower respiratory tract infections is deciding whether antibiotics are needed and which antibiotic class to choose for treatment of lower respiratory tract infections. Accordingly, the choice of drug will depend on the site of infection, the extent of the disease, the lower respiratory tract inflammation in children or adults as well as the presence of any other underlying disease, history of reaction to medication and patient compliance to achieve optimal infection control.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.