This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Gastrointestinal manifestations of IgA-Henoch-Schonlein vasculitis commonly occur in 50–75% of patients (adults) with abdominal pain and bloody diarrhea. Gastrointestinal symptoms commonly present in patients with IgA vasculitis, although uncommon in adults, are more severe and often atypical. Gastrointestinal symptoms vary in intensity and a cautious laparotomy is required to rule out an acute abdominal condition.
1. What is iga-henoch-schonlein vasculitis?
iga-henoch-schonlein vasculitis formerly known as schonlein-henoch purpura. The etiology of this disease remains uncertain, but immune complexes of IgA and unidentified antigens appear to have a central pathogenic role.
Gastrointestinal manifestations of schonlein-henoch vasculitis are commonly seen and vary from mild to severe, sometimes gastrointestinal symptoms (colic pain, nausea, vomiting, diarrhea, gastrointestinal bleeding) is the first manifestation of the disease. Vasculitis immunoglobulin is usually a self-limited disease with a benign course and treatment usually symptomatic. In severe cases, corticosteroids are needed.
2. Clinical manifestations of schonlein-henoch . vasculitis syndrome
Iga-henoch-schonlein vasculitis often has symptoms such as:
Initially, the patient has a headache, loss of appetite, fever. After that, many symptoms can develop such as rash (especially in the legs), abdominal pain and vomiting, joint pain (especially in the knees and ankles), edema under the skin, edema of the testicles. complete. Clinical diagnosis is easily made when all of these symptoms are present but can be missed when the clinical picture is incomplete; In the absence of classic purpura, the diagnosis of Ig A vasculitis may not be clear.
Purpura and joint pain are often the main symptoms on admission, but symptoms can develop over days to weeks and can vary.

3. Gastrointestinal manifestations of IgA-Henoch-Schonlein . vasculitis
Gastrointestinal involvement occurs in 50–75% of patients (adults) with abdominal pain and bloody diarrhea. Gastrointestinal symptoms commonly present in patients with IgA vasculitis, although less common in adults, are more severe and often atypical. Gastrointestinal symptoms vary in intensity and a cautious laparotomy is required to rule out an acute abdominal condition. Gastrointestinal manifestations range from mild nausea, vomiting, abdominal pain, paralytic ileus to severe gastrointestinal bleeding, intussusception, intestinal ischemia with secondary necrosis, intestinal perforation.
Gastrointestinal symptoms are often the most debilitating manifestation of the disease, they are often seen in young patients. Gastrointestinal manifestations may herald the onset of IgA vasculitis or develop later in the course of the disease. Usually, gastrointestinal symptoms develop within 8 days of rash appearance, although longer durations (weeks, even months) have been described. In 10-15% of cases, gastrointestinal symptoms precede skin manifestations, making differential diagnosis from other causes of acute abdomen more difficult. Rarely, gastrointestinal symptoms may appear without purpura on the skin at any time.
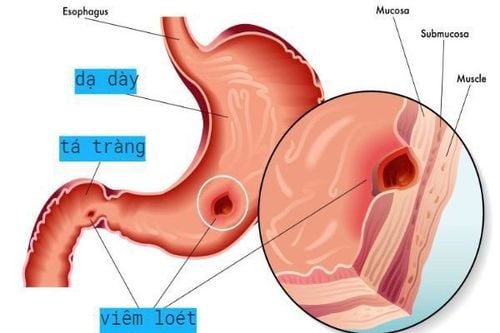
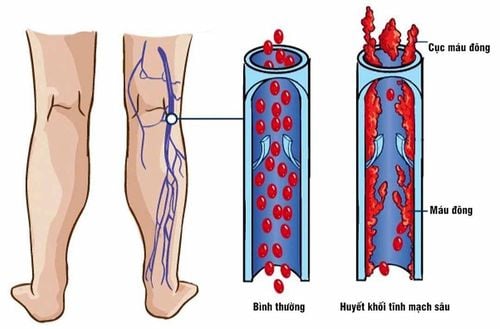
Abdominal pain is the most common gastrointestinal symptom, manifested by food-related cramping pain (similar to intestinal colic), localized in the epigastrium and peri-abdominal region. The pain is thought to be due to the involvement of vasodilating circulation (mesenteric vasculitis) with intestinal ischemia and gastrointestinal edema. IgAV-associated abdominal pain is caused by submucosal hemorrhage and edema.
Abdominal pain is often associated with bloody diarrhea, nausea, vomiting, constipation, and gastrointestinal bleeding (vomiting or melena). In most cases, on physical examination, the abdomen is tender and slightly distended, rarely mimicking and confusing an acute abdomen requiring surgical evaluation (suspected perforation, intussusception).
These cases require urgent computed tomography (CT) scans or unnecessary surgery. Occasionally, especially in younger patients, severe abdominal pain may suggest acute appendicitis, especially in the absence of a skin rash. Even if a rash is present (suggested in the clinical setting for Ig A vasculitis) preceded by severe abdominal pain, the differential diagnosis of abdominal pain and the exclusion of acute surgical abdomen is imperative. Furthermore, the IgA vasculitis rash may be congestive or urticarial, nonspecific or limited to lesions of the buttocks and lower extremities in the early stages of the disease.
Gastrointestinal bleeding is another symptom, with prevalence varying from 17.6 to 51%. In most cases, bleeding is occult (detected as positive fecal occult blood) when present, the main symptom being melena rather than vomiting or hematuria, as bowel lesions are often local reside in the small intestine and colon. Gastrointestinal bleeding is usually mild, in rare cases can be severe, requiring blood transfusion or surgical treatment, even leading to death.
Other rare gastrointestinal manifestations such as:
Esophageal ulcers Pancreatitis Pseudomembranous colitis Involvement of the gallbladder Intestinal perforation and ischemic vasculitis. Intussusception is the most common gastrointestinal complication of iga-henoch-schonlein vasculitis. Edema and hemorrhage may act as a pathological guide, contributing to the development of intussusception. Intussusception is limited to the small intestine in about 60% of cases, in contrast to idiopathic, typically ileocolic, intussusception. The overall incidence of this complication of IgA vasculitis varies between 2.3 and 3.5%, although some retrospectives have reported rates as low as 0.4 to 0.6%. Children who have severe gastrointestinal pain or require hospitalization are at higher risk.
4. Visual assessment of gastrointestinal manifestations
Upper gastrointestinal endoscopy (UGD) is mandatory in patients with gastrointestinal bleeding. UGD is useful in the diagnosis of iga-henoch-schonlein vasculitis, particularly when gastrointestinal symptoms develop before skin lesions.
The most important part of the upper gastrointestinal tract involves the second part of the duodenum with endoscopic features, including diffuse mucosal redness, petechiae, severe erosive duodenitis, hemorrhagic lesions and ulcers. Pyloric lesions may be seen on endoscopy, usually in the duodenum, stomach, and descending colon.
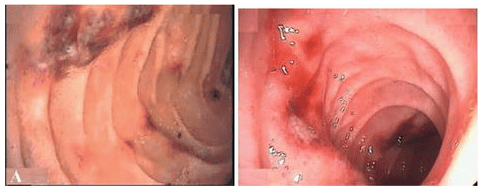
Level of endoscopic findings based on severity of vasculitis. Usually, irregular nodular lesions, ulcers, or hematoma-like protrusions are characteristic of iga-henoch-schonlein vasculitis of the duodenum. The stomach and colon are also commonly affected, but the duodenal bulb is rarely affected, and the absence of duodenal bulbous lesions is important to rule out the etiology of gastrointestinal bleeding.
Biopsy of gastrointestinal lesions is usually done in patients with or without suspected IgA vasculitis to rule out infection, inflammatory bowel disease, and less commonly vasculitis. Biopsy should be obtained before starting steroid therapy, if possible.
Other imaging evaluations of the gastrointestinal tract include:
Colonoscopy: Mucosal congestion, petechiae, and ulcers are the most common findings. Computed tomography (CT) image: The telltale signs of IgA vasculitis are multifocal symmetry, circumferential, regular wall thickening and distension of the mesenteric vessels. Related findings include free intraperitoneal fluid, affected loops of ileum, vascular occlusion in the adjacent mesentery, and nonspecific lymphadenopathy. The target sign is not specific, it can be encountered in many other diseases such as intestinal ischemic disease, inflammatory bowel disease, infectious enteritis, radiation enteritis,... In some cases Selectively, CT angiography may be used to visualize the location of arterial or venous occlusion. However, a normal angiogram does not rule out the possibility of mesenteric ischemia. Areas of obstruction and mesenteric vessels are also seen in Crohn's disease, but involvement of the terminal ileum, stenosis, fistula, and abscess favors Crohn's disease over other conditions.
5. Conclusion
Diagnosis of IgA vasculitis (HSP) is usually based on clinical manifestations of the disease and, in patients with incomplete/abnormal presentation, biopsy of the affected organ (eg, skin or kidney) for Predominantly IgA deposition supports the diagnosis. Although gastrointestinal involvement is frequent, the diagnosis of IgA vasculitis can be difficult when gastrointestinal manifestations occur singly or precede the appearance of the characteristic cutaneous purpura.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Camelia Cojocariu, Ana Maria Singeap,Gastrointestinal Manifestations of IgA Vasculitis-Henoch-Schönlein Purpura, December 4th2018. https://www.intechopen.com/