This is an automatically translated article.
Cholecystoduodenal fistula is an abnormal passage between the bile duct system and the digestive tract that occurs spontaneously. In other cases, gallbladder fistula is a rare complication of untreated gallstones. These gallbladder fistulas cause a variety of clinical presentations and can be life-threatening.
1. What is a gall bladder or duodenal fistula?
Gallbladder fistulas are chronic bile duct-like ulcers between the gallbladder and adjacent viscera. They may connect the gallbladder to the bile duct system but rarely involve the gastrointestinal tract (internal fistula) and abdominal wall (external fistula). Thus, a cholecystoduodenal fistula is when there is a connection between the gallbladder and the duodenum, which is the site of bile secretion into the digestive tract of the common bile duct.
In the class of cases, gallbladder fistula is a rare complication of cholelithiasis or neoplastic lesions and is classified as primary or secondary. For internal fistulas, such as cholecystoduodenal fistulas, the cause is usually inflammatory and mainly occurs as late complications of gallstone disease or tapeworm infection. On the other hand, biliary tract interventions such as laparoscopic cholecystectomy can also cause secondary gallbladder fistulas.

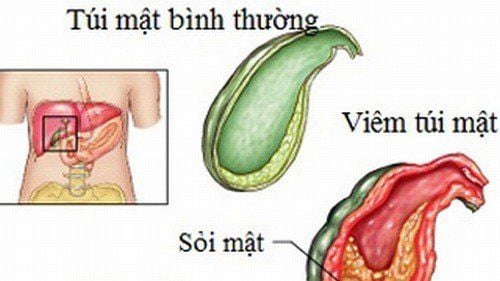
Túi mật bị rò là biến chứng hiếm gặp của bệnh sỏi đường mật hoặc các tổn thương tân sinh
2. How to diagnose gallbladder duodenal fistula?
Preoperative diagnosis of gallbladder or biliary fistula in general and cholecystoduodenal fistula in particular is still challenging and is achieved only in 8–17% of cases. Patients often present with a history of biliary stones, including common symptoms such as persistent right upper quadrant abdominal pain, abdominal cramps that increase after meals, gastrointestinal disturbances causing nausea, bloating, or difficulty in swallowing. diarrhea and Mirizzi Syndrome may also be present.
One factor suggesting the possibility of gallbladder fistula is when the patient has a history of previous surgical intervention on the biliary tract. At this point, in order to best plan the diagnosis and complete treatment, the physician should identify the following characteristics:
Cause of gallbladder fistula : Presence of gallstones, this is a condition most frequently encountered etiological condition. In the absence of stones, look for other inflammatory conditions or cancer; The degree of obstruction of the biliary tract and the presence of erosion or destruction of the gallbladder wall; Presence of bilateral fistula. Commonly indicated laboratory tests to evaluate the above features include:
Abdominal ultrasonography is a non-invasive diagnostic tool that is easily performed to demonstrate the presence of gallstones; Magnetic resonance cholangiopancreatography (MRCP) has better diagnostic accuracy (about 50% of cases) as well as provides better information on the anatomy of the bile duct system and gallbladder. Accordingly, the degree of obstruction is easily demonstrated by CT. Furthermore, the tool is also useful to exclude neoplastic lesions located in the hilum or in the liver parenchyma with invasion of the gallbladder; Invasive procedures, such as endoscopic ultrasonography and endoscopic retrograde cholangiopancreatography (ERCP) have higher diagnostic accuracy for detecting cholecystoduodenal fistulas or all gallbladder fistulas. In particular, ERCP has high accuracy when it is necessary to identify the primary biliary fistula, and also has the role of both treatment and surgical intervention, which is stone removal after sphincterotomy and stenting. bile duct.

Sự hiện diện của sỏi mật là nguyên nhân của rò túi mật
3. How to treat gallbladder duodenal fistula?
Gallbladder and duodenal fistula can only be resolved by surgical intervention. However, surgical treatment of primary biliary fistula remains a challenge for most surgeons.
Accordingly, surgeons always require a good knowledge of pathology, lesions on the bile duct system and the relationship of different organs in the gastrointestinal tract. Inflammation in Calot's triangle often causes significant anatomical changes in the hilar region and can make it difficult for surgeons to manage intraoperative lesions.
The basic principle of cholecystoduodenal fistula surgery is reconstruction of biliary drainage, usually including cholecystectomy, duodenal reconstruction and a combination of stone removal, dissection of the compression or tumor. as well as eliminate the inflammatory foci of infection. Depending on the situation, personal experience of the surgeon or available facilities, the patient will be considered for interventional cholecystectomy, retrograde cholecystectomy, laparoscopic surgery or open laparotomy.
After surgery, the patient can be placed a biliary drainage tube to ensure the best possible recovery of the structure and function of the biliary system. An peritoneal tube may also be left if there is uncontrolled inflammation in the abdomen. However, these tubes will be removed before the patient is discharged from the hospital. After that, the patient still needs to be periodically monitored, evaluated postoperatively and performed imaging tests as prescribed by the doctor to determine the success of the surgery, excluding possible complications.
In summary, a cholecystoduodenal fistula is an uncommon fistula between the gallbladder and duodenum. This condition often occurs when there are causes of chronic cholecystitis, often due to stones. The diagnosis was primarily using ultrasound imaging and was later confirmed by computed tomography. The main treatment is surgery and patients need to monitor and prevent recurrence later.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: revistagastroenterologiamexico.org, ncbi.nlm.nih.gov, adiopaedia.org