This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
EMR techniques in gastrointestinal polypectomy can be divided into aspiration and cutting (aspiration) or lifting and cutting (non-aspiration) techniques. However, in certain cases, both techniques are used together.
1. Make a problem
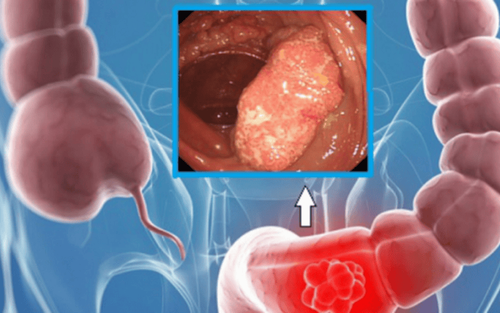
Many gastrointestinal cancers are diagnosed at an advanced stage, requiring major surgery which is associated with significant morbidity and mortality. The outcome of these cases is suboptimal due to local or distant metastasis. Endoscopic mucosal resection was developed in Japan for the management of early gastric cancer. This has become more widely accepted as a treatment option for various gastrointestinal lesions globally.
Indications have expanded to include the treatment of Barrett's dysplasia, esophageal squamous dysplasia, small bowel and colorectal adenomas. Endoscopic mucosal resection (EMR) also has the advantage of providing data for more accurate local staging of the disease compared with ablative therapies, such as argon plasma ablation (APC), therapy photodynamic or radiofrequency ablation (RFA). However, gastrointestinal polypectomy requires adequate expertise and training to be safe and effective.
2. Morphological classification of superficial tumors
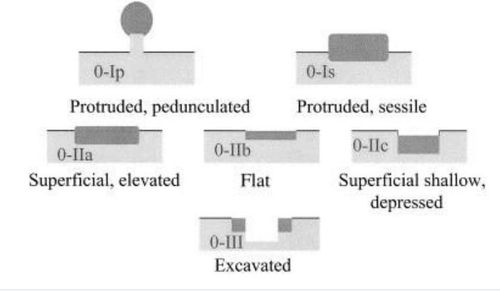
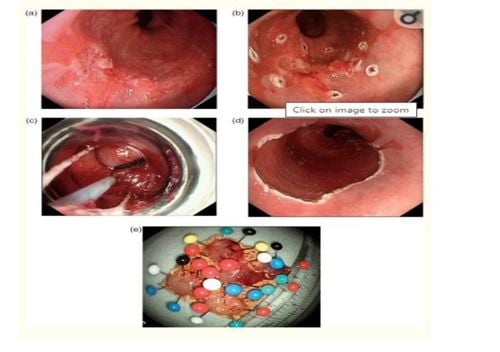
Neoplastic lesions in the gastrointestinal tract are said to be superficial when their endoscopic findings suggest that invasion is limited to the mucosa and submucosa. The Japan Society of Stomach Cancer has developed a guide to classifying advanced gastric cancer from types 1-5. Then, category 0 was added to describe superficial lesions.
Type 0-I is further subdivided into pedunculated (0-Ip) and sessile (0-Is) lesions. Type 0-II is divided into three sub-categories; 0-IIa indicates a slightly elevated lesion, 0-IIb represents a flat lesion, and 0-IIc represents a concave lesion. Type 0-III is a concave lesion. Various combinations of this classification may be used to describe mixed lesions that are tall, flat, or concave.
For example, a flat and concave, non-convex, non-scarring lesion is described as type 0-IIb/c. Although these manifestations have been mainly described in gastric cancer, the same classification was adapted for superficial lesions of the esophagus and large intestine. In type 0-I lesions, diameter is a reliable predictor because the risk of submucosal invasion increases with diameter. However, with type 0-II lesions, the morphological subtypes are of greater importance. Invasion of the submucosa is more frequent in concave lesions (0-IIc). The rate of submucosal invasion is high in type 0-III lesions. Staining endoscopy and advanced optical or electronic imaging technologies such as narrow band imaging (NBI) will be helpful to characterize these lesions.
3. Stage of lesions
Accurate in situ staging would be ideal prior to performing EMR in gastrointestinal polypectomy. However, this is not easy to achieve in many cases. Computed tomography (CT) is performed to exclude distant metastases and various studies have shown that distant metastases are almost non-existent in cancers confined to the mucosa. A prospective study of 100 patients with Barrett's early cancer showed that CT did not affect TNM classification. However, the risk of metastasis is increased with submucosal invasion and in these cases.
Endoscopic ultrasonography (EUS) is a very accurate tool for T and N staging of advanced esophageal cancer. However, its value in early neoplasia is questionable. EUS standard resolution is not sufficient to differentiate superficial mucosal tumors from deeply invasive tumors. However, EUS is useful in N segmentation and accuracy is greatly improved (90%) by the addition of fine needle aspiration (FNA). A retrospective study of the role of high-resolution endoscopy (HRE) and EUS in 50 patients with Barrett's early neoplasm showed that Paris 0-IIa or 0-IIb lesions were associated with mucosal disease (83–100%) compared with the Paris classification 0 -IIc lesions (66%), where invasion of the submucosa is more likely.
Another prospective study compared HRE with high resolution EUS in early esophageal cancer. The results of this study demonstrated that the overall diagnostic accuracy of HRE and high-resolution EUS was high (approximately 80%), with no significant difference between the two techniques. However, the diagnostic accuracy is unsatisfactory, especially in distinguishing mucosal disease from submucosal disease. A small EUS probe with frequencies up to 20–30 MHz is needed to differentiate mucosal and submucosal layers, but results are not entirely satisfactory. For gastric carcinoma, the accuracy of detecting sm1 infiltration was 65–79%.
4. Histological evaluation
One of the most important prognostic factors of lymph node metastasis is the infiltration of the lesion. Mucosal lesions are subdivided into T1m1, where disease is limited to the superficial epithelial layer, T1m2 where the disease involves the lamina propria, and T1m3 persists as well as involving mucosal muscles. Similarly, submucosal involvement is further subdivided into T1sm1, T1sm2, and T1sm3, as evidenced by the involvement of the superficial one-third, the middle third, and the deepest one-third of the submucosa. The incidence of mucosa-associated lymph node metastases is negligible (T1m1-m3) and thus these lesions may be suitable for endoscopic management, whereas those involving submucosal The fascia increases the likelihood of lymph node metastasis, ranging from 0–8% in T1sm1 to 26–67% in T1sm2–3 lesions. Therefore, deep submucosal invasion is considered an indication for surgery and EMR in gastrointestinal polypectomy to determine the exact local location.
5. Endoscopic cutting technique
EMR techniques for gastrointestinal polypectomy can be divided into aspiration and cutting (aspiration) or lifting and cutting (non-aspiration) techniques. However, in certain cases, both techniques are used together. In the lift and cut technique, a submucosal injection is used to separate the muscle pad from the lesion and this reduces the risk of perforation. In the case of an invasive lesion, a sign of failure to elevate the lesion that becomes apparent after submucosal injection is the possibility of further invasion of the lesion, thus making it impossible to perform an EMR. Colonic EMR is usually performed without aspiration and using a noose to remove polyps after submucosal injection.
6. Solutions used
Various solutions are used for submucosal injection. Regular saline is the most widely used agent, but it is absorbed quickly. To overcome this, it is common to use other agents such as hypertonic saline, 50% dextrose, sodium hyaluronate, 4% succinylated gelatine, etc. Injections are made with a needle at one or more pulse sites. around the injury.
7. Indications for endoscopic mucosal resection in early stage gastrointestinal cancer.
Table of indications for endoscopic mucosal resection for early stage gastrointestinal cancer: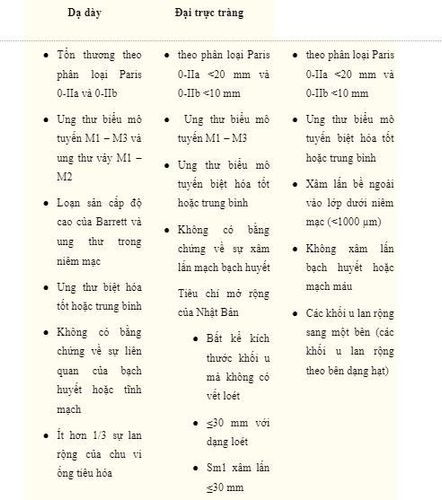
8. EMR is particularly useful in the management of large pedunculated and flat lesions of the colon.
Polyps larger than 2 cm can be cut in segments to avoid perforation. However, there are concerns regarding incomplete histological evaluation and higher recurrence rates after partial resection. In 148 cases of large and giant polyps, EMR was performed blockwise in 44% of cases and partial in the rest. The recurrence rate was 4.2% after a median follow-up of 30 months.
A second study included 186 endoscopically resected polyps with a maximum diameter of 3 to 13 cm. Of the 141 pedunculated polyps that were resected, two patients had surgery because of intraprocedural bleeding and one patient because of late cecal perforation. During a median follow-up of 40 months, only 3% of patients relapsed to a benign disease. However, a recent meta-analysis including 25 studies found a lower composite rate of curative complete resections at 59%. According to studies, the polyp recurrence rate after total resection is 60% less than partial resection and the additional use of APC does not improve the recurrence rate. However, an earlier randomized trial showed that polyp recurrence after complete resection of large polyps was significantly reduced with the use of APC.
9. Complications of gastrointestinal polyp removal
Bleeding and perforation are the main complications associated with EMR in gastrointestinal polypectomy. In cases of transesophageal EMR, there was no difference in complications when the EMR technique was compared with ligation and excision. Of the 100 EMR cases, only two patients had mild bleeding and no perforation.
A mucosal defect involving more than 3/4 of the circumference of the esophagus after EMR was significantly associated with the subsequent development of esophageal stricture. Bleeding is the most common complication occurring in 7–8% of patients receiving standard EMR or ESD treatment for EGC. Perforations were uncommon in gastric EMR compared with ESD (4%). High doses of proton pump inhibitors are usually given for 4-8 weeks to facilitate mucosal healing following upper GI EMR. Patients are usually given fluids only for 24 hours, followed by a soft diet for 3 days.
Injecting an adequate amount of submucosal fluid is paramount to avoid colonic perforation, especially in right-sided lesions. A recent series of colonic EMR techniques in 182 lesions showed a rate of perforation in 1% and bleeding in 12%. Minor and more frequent complications include post-polypectomy pain and syndrome.
10. Conclusion
EMR is an important advance in the field of therapeutic endoscopic therapy and has been accepted as a minimally invasive alternative to surgery in mucosal lesions affecting the upper and lower gastrointestinal tract. The greatest experience has been mainly from Japanese endoscopists, but the indications have been expanded to include predominantly Western diseases such as Barrett's esophagus. EUS may be useful to assess the nodal stage of early cancer. However, its role in differentiating mucosal and submucosal cancers is questionable. Endoscopic morphology is a useful guide for evaluating lesions that may be suitable for EMR. These procedures carry a high risk of complications and should be performed by trained and experienced endoscopists.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Jayan Mannath , MD, MRCP, Endoscopic mucosal resection: who and how? Therap Adv Gastroenterol. 2011 Sep; 4(5): 275–282.