This is an automatically translated article.
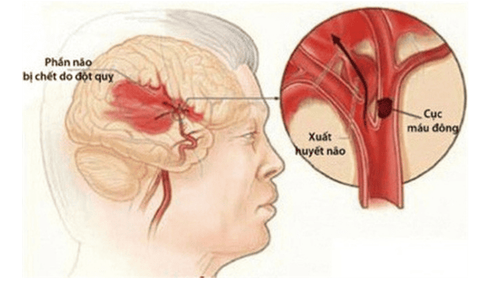
While the subacute and long-term treatment of patients with stroke involves only physical therapy and finding the exact cause of the event to prevent recurrence, it makes sense to treat acute stroke. improve long-term prognosis, including quality of life later in patients. Accordingly, the immediate goals of acute stroke management include rapidly minimizing brain damage, treating medical complications, and minimizing patient symptoms on a pathophysiological basis.
1. Detecting and sending acute stroke patients to hospital
The detection and hospitalization of an acute stroke patient depends on the following factors:
Sudden onset of CNS defects Presence of new neurological deficits Degree of brain damage above Imaging Inquiry for investigation of stroke causes Comorbidities and need for personal care support Suspect stroke as a result of serious underlying disease such as bacterial endocarditis Most stroke specialists recommend hospitalization for acute stroke, but there may be circumstances that may not benefit the patient. For example, a dementia patient with a recent history of gastrointestinal bleeding, who is living in a nursing home, may be better off in a nursing home than being hospitalized. Furthermore, in patients who are not eligible for any antithrombotic treatment, hospitalization or even cranial computed tomography is of little value.

Người bệnh đột quỵ cấp cần được nhanh chóng đưa tới cơ sở y tế
2. General management of acute stroke treatment
There is now ample evidence that stroke unit care gives patients the best chance of independent survival. Out of every 100 patients treated, there will be only 40 independent survivors with non-specialized general care, but as many as 46 independent survivors if admitted to a stroke unit. Even this increase (additional six independent survivors) is two to three times more effective in thrombolytic therapy for acute myocardial infarction.
The comprehensive benefit in the overall management of acute stroke treatment is due to the agglomeration and accumulation of many small effects performed by a team of nurses, paramedics and stroke physicians as well as multidisciplinary staff for total dependent care.
Overall, general interventions for acute stroke include appropriate rehydration, early mobilization, thorough investigation of stroke causes, rehabilitation; At the same time, attention should be paid to diet, swallowing capacity, and the prevention of DVT in patients who are likely to be immobilized for long periods of time.
3. Medical indications in the treatment of acute stroke
Drug therapy includes aspirin, thrombolytics, and antihypertensives. In contrast, anticoagulants, neuroprotectives, steroids, mannitol, and glycerol have been shown to be ineffective or harmful in the acute stroke phase.
Aspirin
An immediate dose of aspirin for ischemic stroke patients certainly works. However, efficacy was modest, with only one additional independent survivor per 100 patients treated. However, if counted across a large population of patients hospitalized for acute stroke, this treatment would prevent several hundred thousand deaths or disabling strokes each year.
In addition, the benefits of aspirin given for two weeks after an ischemic stroke are the same as those seen over the next 50 weeks, to prevent the likelihood of a secondary stroke occurring more often. regulation. This is based on evidence from a series of recurrent ischemic strokes within the first few weeks after the stroke or transient ischemic attack.
Người bị đột quỵ do thiếu máu cục bộ có thể dùng Aspirin dưới sự hướng dẫn của bác sĩ
Thrombolytics
Recombinant tissue plasminogen activator (rt-PA) is therapeutic to improve approximately 10-15 independent survivors per 100 treated patients. Meanwhile, this method could not avoid the undesirable outcome of an additional 8 patients with symptomatic intracerebral hemorrhage. At the same time, this indication has not yet been shown to have a definite impact on its ability to improve overall mortality. Furthermore, thrombolytics are still not always available at primary care centers without a stroke specialist.
In addition to one, another factor that makes access to thrombolytic therapy difficult is that it is indicated only for patients who can be evaluated, radiographically examined and will be followed up, treated by an experienced stroke team within three hours of onset. Because this deadline can be difficult to meet, trials are underway to expand the indication "window" and assess whether treatment at a later time point is still safe and effective. In general, however, the current use of thrombolytics in acute stroke management does not have the potential to affect public health, while further investigation is needed for its promise. for some patients to arrive early in the "golden time".
Blood pressure stabilizers
The effect of antihypertensive drugs in the acute phase of stroke is uncertain. Some experts tend to prefer treatment of patients with persistently very high blood pressure (greater than 180/120), especially those with primary intracranial hemorrhage, in order to maintain blood pressure. cerebral perfusion.
In cases where the patient's blood pressure rises above this threshold, treatment will be considered necessary and oral therapy with conventional antihypertensive drugs may be used. For patients with difficulty swallowing due to acute brain damage, the drug can still be administered orally through a nasogastric tube or using parenteral blood pressure stabilizing drugs.
Reversal of antithrombotic effects
Antiplatelet therapy should be discontinued immediately, possibly indefinitely, if the stroke is due to primary internal bleeding. If a patient on anticoagulation has a primary intracerebral hemorrhage, urgent evaluation and consideration should be given to hematologists to reverse anticoagulation.
Thereafter, anticoagulation should not be reintroduced unless the patient is at high risk of major thromboembolism such as a history of metal prosthetic heart valve replacement.
4. Surgical treatment in acute stroke
Indications for surgical intervention will be considered for the purpose of reducing the risk of acute cerebral edema due to posterior fossa stroke. Accordingly, craniofacial opening can sometimes save the lives of acute stroke patients by reducing intracranial pressure secondary to large hemispheric infarction.
However, an early intervention trial of hematoma aspiration for people with primary intracerebral hemorrhage did not show any benefit.

Bác sĩ có thể lựa chọn phương pháp phẫu thuật trong đột quỵ cấp
5. Adaptive skills support for patients and carers
Acute stroke can be seen as a serious problem for not only the patient but also carers and families. Accordingly, relatives need to be supported and provided with information at this important time.
By assessing severity and based on the classification of stroke types, doctors can make estimates of prognosis. For example, patients who present with hemiplegia and aphasia have a 90-95% chance of dying or being disabling after six months, with a worse prognosis for most cancers. In contrast, if the patient had only an acute stroke with dyskinesia, the mortality rate would be lower, but there would still be a 30% chance of long-term disability.
In addition, some instructions on returning to life such as driving, working... are also meant to support life reintegration, including important legality.
In summary, acute stroke is a serious cerebrovascular event that occurs suddenly with a very high mortality and disability rate. However, the patient's prognosis is partly dependent on the initial steps of acute stroke management. Thereby, it is necessary to quickly detect signs of stroke and bring patients to emergency centers, especially where stroke units are located, in order to improve outcomes afterwards.
Periodic health checkup is one of the ways of early recognition and prevention of disease, especially for patients with a history of stroke, from which a treatment plan can achieve optimal results. Currently, Vinmec International General Hospital has general health checkup packages suitable for each age, gender and individual needs of customers with a reasonable price policy, including:
Health checkup package diamond general health checkup package Vip general health checkup special health checkup package Comprehensive general health checkup package standard general health checkup The patient's examination results will be returned to your home. After receiving the results of the general health examination, if you detect diseases that require intensive examination and treatment, you can use services from other specialties right at the Hospital with quality treatment and services. outstanding customer service
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: ps.org.au