This is an automatically translated article.
The article is written by Master, Doctor Mai Vien Phuong - Gastroenterologist - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
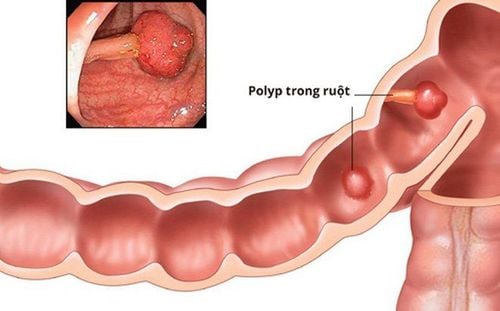
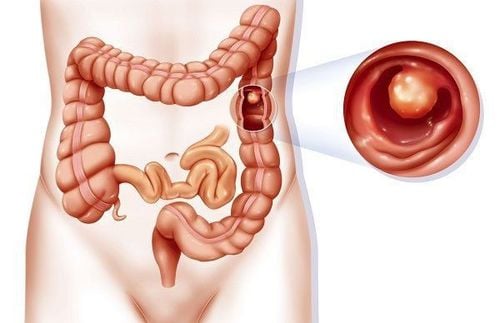
Polypectomies are polypectomy procedures performed during laparoscopic surgery that are generally safe. The most feared complication of this method is colonic perforation, which is manifested by symptoms of acute peritonitis after colonoscopy. A lesser known entity, post-polypectomy electrocautery syndrome, should be considered in the differential diagnosis when a patient presents with acute postoperative abdominal pain.
1. Presenting the clinical situation
A 78-year-old man with a history of coronary artery disease presents to the emergency department with fever and abdominal pain 5 hours after laparoscopic colon polypectomy of the cecum. Although he initially tolerated the procedure well, the history noted the development of a diffuse, intermittent abdominal pain upon return home, which resolved with the cessation of bloating. A few hours later, he presented with severe right lower abdominal pain, aggravated by coughing and movement with no significant remission factors. The patient refuses nausea, vomiting, or a change in bowel habits.
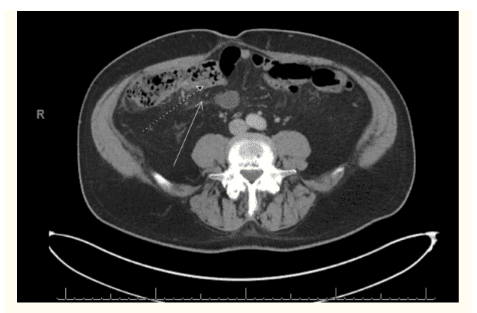
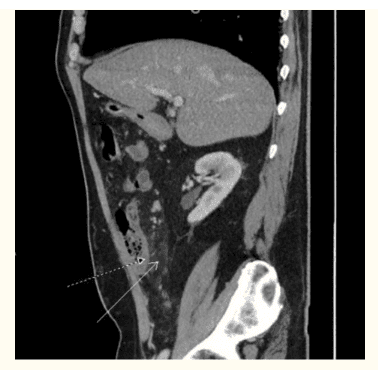
On examination, the patient's temperature was 38.1°C with the remaining vital signs within normal limits. On abdominal examination, the patient had normal bowel sounds with diffuse pain, most pronounced in the right lower quadrant. There is no peritoneal sensation or abdominal stiffness like wood. Tests revealed a white blood cell count of 19,000 cells/mcL (reference range: 4,800–10,800 cells/mcL). The patient's serum lactate was 1.9 mmol/L (reference range: 0.5–2.2 mmol/L). Abdominal radiographs were considered normal. Contrast CT of the abdomen and pelvis showed significant inflammatory changes in the mesenteric fat around the cecum and thickening of the cecum wall.
The patient was evaluated by the department of gastroenterology and general surgery, who attributed his symptoms to post-polypectomy electrocautery syndrome, with acute postoperative abdominal pain. He was treated conservatively with intravenous fluids, piperacillin/tazobactam 3,375 g every 8 hours and a clear liquid diet.
The patient's acute abdominal pain resolved within 48 hours and was discharged home on a normal diet, taking amoxicillin/clavulanate 875–125 mg tablets twice daily to complete a 5-day course of antibiotics. The patient's symptoms completely resolved on follow-up examination.
2. Discussion
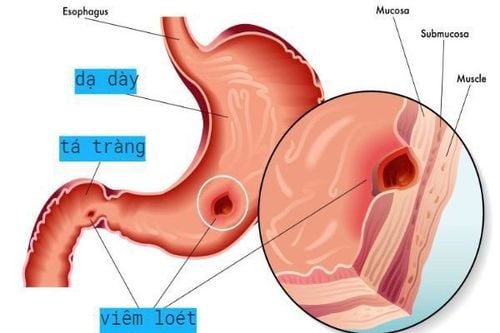
Post-polypectomy syndrome, also known as post-polypectomy syndrome, transdural burn syndrome, or microcomplication, has a reported incidence that varies from 0.003 - 1% in various studies. It results from electrocautery damage to the colonic mucosa and underlying muscle, causing transmural burns with peritonitis but no evidence of colonic perforation on imaging studies. In a large multicenter study, risk factors associated with electrocautery syndrome after polypectomy included: sessile polyp lesion, large lesion size (> 2 cm), right colonic involvement ( due to decreased wall thickness of the right colon) and increased blood pressure. Endothelial dysfunction and atherosclerosis are also considered risk factors by some authors.
3. Time of occurrence of acute abdominal pain due to electrocautery syndrome after polypectomy
Patients with post-polypectomy electrocautery syndrome usually present within 12 hours of endoscopy with fever, tachycardia, and acute generalized abdominal pain. However, the onset of symptoms may be delayed up to 5–7 days after the procedure. Some authors believe that fever after polypectomy of the stomach or colon,... is an unexplained fever that may be a mild version of the post-polypectomy electrocautery syndrome.
4. Clinical examination
Abdominal examination in patients with post-polypectomy electrocautery syndrome can identify pain at the polypectomy site, with 20% of cases presenting with resistance and abdominal spasticity. Laboratory tests that may show leukocytosis add to the suspicion of colon perforation. CT scan of the abdomen and pelvis is the diagnostic modality of choice to distinguish post-polypectomy electrocautery syndrome from colonic perforation. In post-polypectomy syndrome, a CT scan shows focal thickening of the colonic wall with surrounding fatty fibers without external air.
Patients with post-polypectomy electrocautery syndrome are usually managed conservatively with intravenous fluids, pain control, gradual increase in diet as tolerated, and with or without antibiotics against Gram pathogens. negative and anaerobic. Less severe cases can be managed in an outpatient setting with antibiotics and fluids for 1–2 days. Symptoms tend to clear up within 2-5 days. For patients who do not improve with conservative measures, immediate surgical consultation is recommended to consider the possibility of potential perforation.
The prognosis of electrocautery syndrome after polypectomy of the stomach, colon,... is generally good, of which 2.9% have major complications (need ICU admission) and 0% die for the study. The study included 34 patients. However, patients with full-thickness burns may have a relatively worse outcome, as necrosis of the bowel wall can eventually lead to late perforation, requiring urgent surgical exploration.
5. Prevention of acute abdominal pain caused by post-polypectomy syndrome
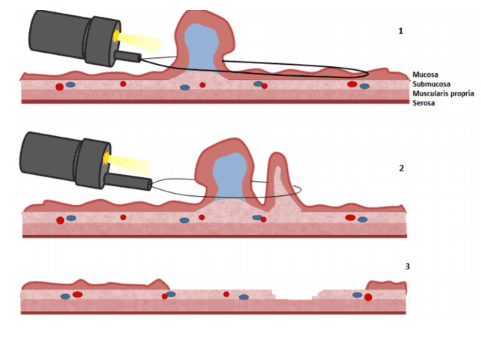
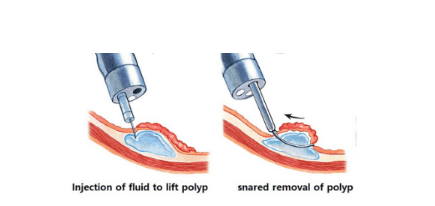
Submucosal injections of various solutions to raise large polyps are often done to try to separate the remaining layers of the colon from damage from electrocautery, especially in more complex cases. associated with larger polyps (>1.5 cm) in the right colon. Right colon polyps are thought to pose a higher risk of colonic injury due to their relatively thinner walls (2–3 mm when inflated with air), especially if electrocautery is used. Techniques using conventional saline injections below polyps with or without epinephrine, sodium hyaluronate, 50% dextrose, and glycerol have all been attempted to protect the underlying colon from injury, however no technique has been used. Which has been shown to be more effective in studies.
In addition, endoscopic technique can influence the probability of complications after the procedure. The use of hot biopsies leads to a significantly higher risk of transmural damage compared with conventional noose polypectomy. Nose polypectomy (electrocautery polypectomy) is commonly used by gastroenterologists for polyps > 7–8 mm. During the removal of pedunculated polyps, the use of early energy and slow closing of the noose one-third or one-half of the way to the base of the polyp can reduce the risk of post-procedural complications. Thermal damage to the colonic wall can also be reduced by directing the polyp toward the center of the lumen, just before the effects of heat, increasing the distance between the submucosa and the lamina propria and serosa. Furthermore, aspiration after placing the noose around the base of the polyp on the thinner right colon can reduce wall tension, increase wall thickness and polyp amplitude, thereby facilitating resection. polyp.
A steel noose can be associated with significantly deeper tissue trauma than a tungsten noose. Therefore, more research is needed on the best and safest techniques for polyp removal.
In summary, in patients presenting with acute abdominal pain, fever, or tachycardia within 12-24 hours after colonoscopy with polypectomy, the physician should consider both perforation and post-polypectomy syndrome. CT scan of the abdomen and pelvis is the imaging technique that can differentiate these two entities.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Asad Jehangir, MD et al. Post-polypectomy electrocoagulation syndrome: a rare cause of acute abdominal pain. J Community Hosp Intern Med Perspect. 2015; 5(5): 10.3402/jchimp.v5.29147.