This is an automatically translated article.
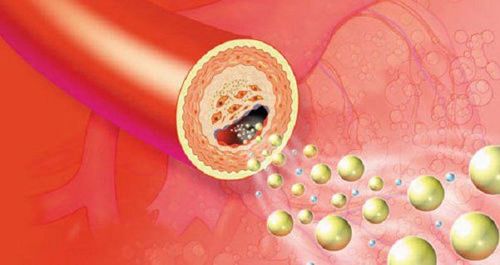
Dyslipidemia is the cause of many dangerous cardiovascular diseases such as atherosclerosis, myocardial infarction,... Diagnosis of dyslipidemia plays an important role in early detection and treatment. timely and effective treatment, avoiding the risk of unpredictable complications.
1. What is dyslipidemia?
Lipid is a substance found in cell membranes, which is the main source of energy for the body (providing up to 25 - 30% of the body's energy needs). Types of blood lipids include chylomicron micronutrients containing triglycerides, VLDL (very low density lipoprotein), LDL (low density lipoprotein) and HDL (high density lipoprotein).Dyslipidemia is a medical condition when one or more lipid parameters are disturbed (elevated LDL-c, raised cholesterol or raised triglycerides, decreased HDL-c). Dyslipidemia is the cause of increased risk of cardiovascular - endocrine - metabolic diseases. Causes of dyslipidemia can be primary, such as genetics or secondary, such as an unscientific lifestyle....
2. Diagnosis of dyslipidemia

Chẩn đoán rối loạn lipid máu thường dựa trên thăm khám lâm sàng và các xét nghiệm máu
2.1. Clinical diagnosis Dyslipidemia is a disease that often has no specific symptoms in the early days of its appearance. Most of the clinical symptoms of this disease are detected only when high levels of blood lipid components persist or cause complications such as atherosclerosis, cerebrovascular accident, myocardial infarction, and jaundice. in eyelids, elbows, knees, acute pancreatitis,...
Characteristic signs in the periphery of the corneal arc: pale white, circular or incomplete, appearing around the iris, pointing hypercholesterolemia,...; Erythema: appearing on the upper or lower eyelids, localized or diffuse; Tendon yellow tumor: appearing in the extensor tendons of the fingers, the Achilles tendon and the position of the knuckles; Subperiosteal jaundice: occurs in the anterior tibial tubercle, on the bony end of the elbow and, more rarely, tendinous jaundice; Jaundice or tubercles: appear mainly on elbows and knees; Palmar pallor form: appears in the folds of the fingers and palms. Characteristic signs in viscera Lipidosis retina: ophthalmoscopy detects retinal lipid contamination in cases of high blood triglycerides; Fatty liver : regional or whole liver infection, detected by ultrasound or computed tomography, often accompanied by hypertriglyceridemia; Acute pancreatitis: common when triglycerides above 10g/L, acute inflammation, subacute edema, blood amylase not increased or moderately increased; Atherosclerosis: is a long-term complication of elevated lipoproteins, often associated with previously unknown elevations of lipoproteins, and may be associated with other risk factors such as smoking and diabetes. 2.2. Subclinical diagnosis Quantifying lipid bilan: because lipid parameters increase after eating, to accurately diagnose dyslipidemia, patients need to draw blood in the morning before eating. Commonly investigated parameters include Blood Cholesterol (TC), Triglyceride (TG), LDL-Cholesterol (LDL-c), HDL-Cholesterol (HDL-c); Diagnosis of dyslipidemia is made when there are some clinical manifestations of the disease such as obesity, yellow rash, coronary artery disease, complications in some organs such as cerebrovascular accident,... Diagnosis is confirmed by testing lipid parameters when there is one or more disorders such as: blood cholesterol > 5.2 mmol/L (200mg/dL); triglycerides > 1.7 mmol/L (150mg/dL); LDL-cholesterol > 2.58 mmol/L (100 mg/dL) and/or HDL-cholesterol < 1.03 nmmol/L (40 mmol/L). The diagnostic criteria for dyslipidemia have undergone many changes with a tendency to gradually lower the normal values of atherosclerotic lipid components (including cholesterol, LDL-c and TG) and increase the normal values. of the anti-atherosclerotic (HDL-c) components.
3. Who should be screened for dyslipidemia?

Người trên 40 tuổi nên xét nghiệm bilan lipid máu định kỳ mỗi năm một lần để phát hiện và diều trị kịp thời nếu bị rối loạn lipid máu
All adults aged 20-40 years should have a fasting lipid bilan test every 5 years; People over 40 years old should have blood lipid bilan test periodically once a year for timely detection and treatment if they have dyslipidemia; People with other cardiovascular risk factors such as diabetes, high blood pressure, coronary heart disease, etc. should be tested earlier and more often depending on the specific case as recommended by the doctor. Diagnosing dyslipidemia helps to detect and treat early complications of the disease. Therefore, if there are risk factors for dyslipidemia, the patient should be examined and diagnosed early to have an effective treatment option.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Compiled source: Department of Preventive Medicine - Ministry of Health