This is an automatically translated article.
The article was professionally consulted by Doctor II Phan Phi Tuan, Head of General Surgery Department, Vinmec Phu Quoc International General Hospital.Peritoneal effusion is an abnormal accumulation of fluid inside the abdomen. In the early stages, patients do not have obvious symptoms, so it is difficult to detect the disease. When the effusion is severe, causing the abdominal skin to stretch with symptoms of tension and discomfort, the patient goes to the doctor and conducts diagnostic tests.
1. Is intra-abdominal effusion dangerous?
Severe peritoneal effusion will cause the skin of the abdomen to stretch, a feeling of heaviness in the abdomen and symptoms such as: shortness of breath, abdominal pain, bloating, vomiting, heartburn, protruding navel... Major level of danger side effects cause it.
In case of portal hypertension due to cirrhosis, patients with peritoneal effusion may have leg edema, men with large breasts, vomiting blood, brain diseases or neurological disorders.
Cases of peritoneal effusion due to cancer or other factors that metastasize to other places can cause patients to have prolonged weakness, severe weight loss.
In the case of peritoneal effusion due to heart failure, the patient may find it difficult to breathe or wheeze.
In the diagnosis of peritoneal effusion there are 3 grades:
Grade 1: mild peritoneal effusion, only seen on CT Scanner and ultrasound. Grade 2: detectable through palpation and percussion. Grade 3: severe peritoneal effusion, directly visible, with sound waves when the fluid changes and moves. The color of the fluid also shows how dangerous the disease is:
If the fluid is clear, colorless: The patient has heart disease. If the fluid is pink: The patient has peritoneal tuberculosis or cancer. If the fluid is lemon yellow: The patient has peritoneal tuberculosis or cirrhosis. If the fluid is cloudy like pus: The patient has purulent peritonitis. If the fluid is milky white and has a jelly-like consistency: The patient has chylous fluid, possibly filariasis or a tumor in the abdomen.
2. How is peritoneal effusion diagnosed?
2.1. Diagnosis of symptoms
Look:
Observe the patient in the standing and lying positions:
In the standing position: the abdomen is sagging, the collateral circulation is clearly visible if it is due to cirrhosis. In the supine position: the abdomen can be observed to be enlarged to the sides, even though the belly button is still protruding, there is collateral circulation if due to cirrhosis, the patient's abdomen does not move according to the breathing rhythm. The fluid is often deposited in low areas. Touch:
In case the condition is mild, the fluid is small, when touching, nothing unusual will be felt. In case of moderate or heavy fluid: touching the abdomen, the abdomen is soft. If there is a lot of translation, it will feel like a balloon. Waves sign: a person holds the edge of the hand lightly on the midline of the abdomen. Meanwhile, the doctor will take one hand to press one side of the abdomen, the other hand will flick or pat the opposite side of the abdomen to feel a wave on the opposite palm. This is called the breaking wave sign. Signs of floating stones: in case there is a tumor in the abdomen or liver, enlarged spleen will show this sign. When the finger is pressed quickly and suddenly against the abdominal wall above the tumor, there is a feeling of being touched back to the finger like a floating ice in water.

Type:
This is a very important method in diagnosing peritoneal effusion.
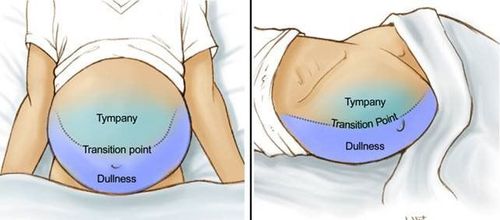
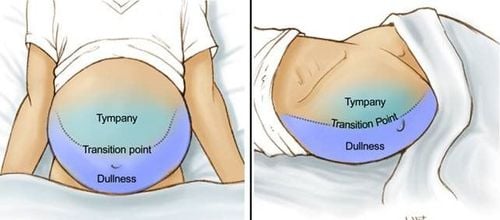
Let the patient lie on his back: knock from the navel to the surrounding positions in the shape of spokes, you will see the area near the navel and the high area has a clear sound, the low area has a dull sound. In case of small ascites, the area with dull sound is only on both sides of the ribs. If there is a lot of ascites, there is a concave curve between the clear and opaque areas. Place the patient in the supine position: doing the same as above will see more opaque areas on the lower side. Combining 3 methods of seeing, touching and percussion can immediately think of ascites if there are signs mentioned above. For a definitive diagnosis, a peritoneal puncture should be performed.
2.2. Peritoneal fluid test
If the patient has an unexplained peritoneal effusion, the peritoneal fluid should be taken for cytology, microbiological culture, albumin measurement, total protein measurement, cytology, and Gram staining. The procedure for testing the peritoneal fluid is as follows:
Observation Most ascites will be clear and slightly yellow in color. There must be at least 10,000 red blood cells/μL for the ascites to turn pink. With at least 20,000 red blood cells/μL, the ascites has a distinct blood red color.
Bloody ascites may have touched the blood vessels during the puncture or may be due to some malignancy. If the fluid is bloody, when the puncture touches the vessel, it will be quite homogeneous and coagulate. If the fluid contains blood that is not due to puncture, the red color is uniform and does not clot because the blood has previously coagulated and subsequently lysed. If the discharge is cloudy and purulent, then an infection has occurred.
Cell count The average ascites contains approximately <500 WBC/μL and <250 polymorphonuclear leukocytes/μL. When an infection occurs, there will be an increase in white blood cells.
If polymorphonuclear leukocytes are > 250/μL, it may be bacterial peritonitis. Lymphocytes often predominate in peritonitis due to metastatic cancer or tuberculosis.
Measurement of differential albumin in ascites and serum This is the best single test to classify peritoneal effusion due to portal hypertension or not due to portal hypertension.
Subtract the albumin value in the serum from the albumin in the ascites. Take care to take the test sample at the same time. The accuracy of this test in classifying ascites is about 97%.

Total protein The classification of ascites as exudative when the protein content is ≥2.5 g/dL is only about 56% accurate in determining the cause of the discharge. Total protein levels combined with measurement of differential albumin in ascites and serum can help to better define the cause.
Culture and Gram staining In the condition that the specimen is immediately injected into blood culture bottles at the hospital bed, the culture has a sensitivity of up to 92% in detecting bacteria in the ascites. Gram staining shows bacteria only in 10% of spontaneous ascites infections when detected early. Detectable by Gram staining requires about 10,000 bacteria/mL. In idiopathic bacterial peritonitis, the mean bacterial density is 1 bacterium/mL.
Cytology In the diagnosis and identification of ascites caused by cancer, smears have a sensitivity of about 58-75%.
2.3. Differential diagnosis
Diagnosing peritoneal effusion with conditions such as:
Large abdomen due to sagging: concave navel, thick abdominal skin, when percussion there is no clear phenomenon above, low opacity. Swollen abdominal skin: Swollen abdominal skin can be identified by pressing a finger against the skin to reveal an indentation. Abdomen is enlarged due to distention: tapping on the abdominal wall does not show signs of crashing waves. Enlarged abdomen due to ovarian cyst: palpating the abdomen can see a tumor. The big belly protrudes upwards, not out to the sides. Enlarged abdomen due to pregnancy: there are signs of pregnancy. Ultrasound shows the fetus. Bladder bridge: there are symptoms of urinary retention, urinary catheterization. For the most peace of mind about the diagnosis of pleural effusion, you should choose a reputable hospital for examination. Vinmec International General Hospital with a comprehensive range of medical qualifications, equipment quality and service quality of international standards is a reliable medical address to perform diagnostic tests.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.