This is an automatically translated article.
Acute pulmonary edema is common in patients with acute or chronic heart disease. If early detection of acute pulmonary edema can save the patient's life, the doctor will have the appropriate diagnosis and treatment.
1. Acute pulmonary edema
Acute pulmonary edema is a state of acute asphyxiation due to many different causes, which causes too much water out of the pulmonary capillaries to cause pulmonary edema. Acute pulmonary edema is an acute, life-threatening disease that can only be saved with early and effective intervention.
Acute pulmonary edema progresses in 3 stages: capillary phase, interstitial phase and alveolar phase. Clinically, acute pulmonary edema corresponds to the alveolar stage. Clinical manifestations are left heart failure, respiratory failure.
Left ventricular failure causes increased left atrial pressure, increased venous pressure and pulmonary capillaries increase capillary permeability, resulting in fluid infiltration into the alveoli, obstructing gas exchange, respiratory failure.
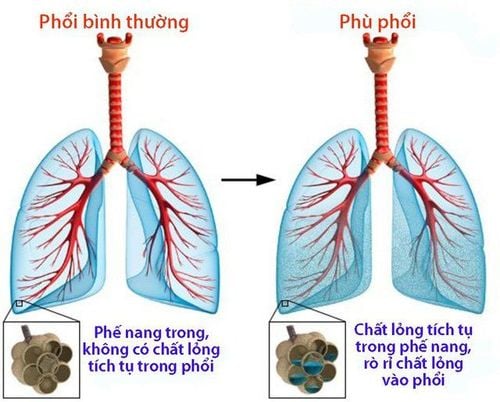
Hình ảnh phù phổi cấp
2. Cause
Due to the imbalance of water exchange between pulmonary capillary, alveolar and interstitial tissues include:
Main factors: increased pulmonary capillary pressure, increased capillary wall permeability. Predisposing factors: decrease in plasma oncotic pressure, lymphatic system occlusion. Depending on the mechanism and pathogenesis, people are divided into 2 types of acute hemodynamic pulmonary edema and acute injury pulmonary edema.
Acute hemodynamic pulmonary edema: is a state of sudden increase in fluid pressure in the capillary lumen that allows plasma to escape into the interstitial and alveolar spaces without anatomical damage to the alveoli. Acute hemodynamic pulmonary edema is often caused by cardiovascular diseases including: valvular heart disease, hypertensive crisis, myocardial infarction, myocarditis. Noncardiac causes such as: acute glomerulonephritis, chronic glomerulonephritis, when pleural effusion procedures are done too quickly or too much or too rapid perfusion. Acute pulmonary edema: is the leakage of plasma fluid through the alveolar-capillary capillary membrane without increasing fluid pressure in the capillary lumen. Acute pulmonary edema lesions due to bacterial, viral, parasitic infections: bronchopneumonia, pneumococcal lobar pneumonia, pneumonic plague, malignant influenza, malignant malaria. Acute poisoning: due to inhalation of toxic substances such as CO2, NO2, SO2, pesticides, strong acids such as gastric juice, corrosive substances, kerosene. Asphyxiation, hypoproteinemia, allergies, anaphylaxis in blood transfusion.
3. Diagnosis
3.1 Ask about the medical history: rheumatic heart disease, congenital heart disease, chronic kidney disease History of oligouria, hematuria and edema, the doctor may suggest glomerulonephritis Sudden heart failure should suggest myocarditis Infusion Rapid fluidization 3.2 Tests The patient needs to do a number of tests including:
Blood count X-ray of the heart and lungs Blood gases Electrocardiogram (ECG) Echocardiogram to diagnose heart disease, evaluate muscle contractility Cardiac Urinalysis Total urinalysis if acute glomerulonephritis is suspected If rheumatic fever is suspected: VS, ASO Troponine, high central venous pressure in suspected myocarditis 3.3 Differential diagnosis Pneumonia: cough, fever, dyspnoea, crackles, chest X-ray shows pulmonary consolidation. Asthma attack : history of asthma attack, lung crackles, chest X-ray shows pulmonary edema. Pulmonary hemorrhage: bloody sputum, no signs of heart failure, no pulmonary edema on X-ray. Acute respiratory distress syndrome: pulmonary edema on chest X-ray, no heart failure.
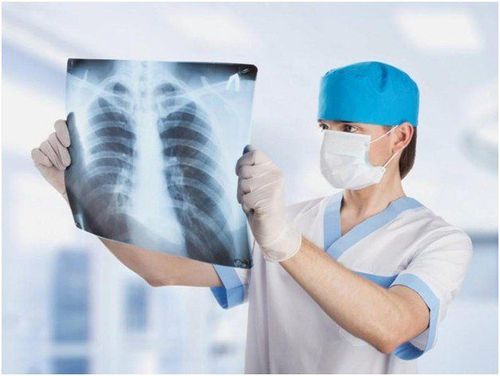
Chụp X-quang tim phổi có thể giúp chẩn đoán bệnh phù phổi
4. Symptoms
4.1 Clinical symptoms 4.1.1 Typical form The typical form is the common form of cardiovascular disease, essentially hypoxia rather than hypercarbia with pallor rather than cyanosis, accompanied by dizziness. sweat, rapid breathing 50-60 times/minute, the patient has to sit up to breathe. Initially, the patient showed a lot of cough, dry cough, then coughed up a lot of pink foam. When the doctor listened to the lungs, there was a small grainy crackle at the bottom of the lung, later on a loud crackle throughout both lung fields. In addition, there may be symptoms of cardiovascular disease such as valvular heart disease, cardiomyopathy, hypertension.
All happens quickly within 15 -30 minutes, if not treated promptly, the patient will die.
4.1.2 The discreet form The discreet form occurs in patients without cardiovascular disease with the following manifestations:
The breathing rate increases gradually, the nostrils rise and fall, the patient struggles and struggles. Distended neck veins. Auscultation of the lungs can be seen as a moist crackle spreading from the bottom of the lung to the top, like a high tide. Asphyxiation leads to coma, cardiovascular collapse, and death. 4.2 Subclinical symptoms Chest X-ray images may have:
Clouds in 2 lungs, concentrated in the hilum and the bottom of the lung. Butterfly-shaped or white lung in OAP lesions. Electrocardiogram helps to diagnose the cause such as myocardial infarction, arrhythmia. Arterial blood gas test: blood pH decreased, SaO2 and PaO2 decreased severely.
5. Treatment
Principles of treatment of acute pulmonary edema:
Reduce blood flow to the heart Respiratory support Drugs that increase myocardial contractility Find and treat the cause: congenital heart failure, rheumatic heart disease, glomerulonephritis 5.1 Acute pulmonary edema Hemodynamics Anti-suffocation: If the early diagnosis is mild, it is necessary to prevent asphyxiation for the patient by having the patient sit with his legs hanging down on the bed. The patient breathes oxygen with a nasal cannula of 6-10 liters/min. In severe form, there is asphyxia, a lot of pink and purple foam, requiring intubation through the nose to suck foam, sputum, squeeze balloons or mechanical ventilation with intermittent positive pressure. Decrease the circulating blood volume with a tourniquet, forcing it moderately to still catch the pulse. Give heart medication Digoxin, diuretic Trofurit, antihypertensive drug if there is hypertension. Sedation may be needed depending on the case. Immediately extract blood if the patient is still having difficulty breathing, extract quickly, more than 300 ml. 5.2 Acute traumatic pulmonary edema Acute traumatic pulmonary edema has a very severe prognosis and requires a longer course of treatment.
Intubation or tracheostomy, mechanical ventilation with continuous positive pressure. Infusion: albumin, plasma if central venous pressure is low, blood pressure is low. Diuretic: trofurite 40-80 mg IV every 4-6 hours. Corticosteroids: methyl prednisolone 40-80 mg every 4-6 hours, or dexamethasone 4 mg, or hydrocortisone 200 mg. intravenous injection. Maintain normal blood pressure. Antibiotic. Patients should be closely monitored for the first 24 hours to prevent recurrence of acute pulmonary edema. Issues to be monitored include:
Pulse, respiratory rate, blood pressure, rales, heart rate, SaO2, jugular vein every 5-15 minutes during the first hour Tri-lime garot monitoring if available Blood gases Specialist examination Cardiovascular to find and treat the cause Acute pulmonary edema is a life-threatening medical emergency if not detected early and treated promptly. Therefore, when seeing abnormal signs, especially for patients with cardiovascular disease, chronic kidney disease, etc., it is necessary for the patient to immediately go to a medical facility for examination and treatment. timely treatment.
Vinmec has a team of respiratory internal medicine doctors with rich expertise and experience in examining and treating diseases related to the respiratory system, especially acute pulmonary edema. Equipped with a system of modern technical equipment according to international standards, Vinmec has been implementing synchronously and effectively the most advanced methods of diagnosis and treatment, bringing trust to both patients and patients. family.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Article referenced source: Vietnam Cardiology Association