This is an automatically translated article.
Article written by BSCK II Nguyen Xuan Thang, Department of Examination & Internal Medicine, Vinmec Central Park International General Hospital
1. WHO 2019: Classification of diabetes
According to WHO 2019, diabetes is divided into several types as follows:
Type 1 diabetes Type 2 diabetes (Type 2 diabetes) Hybrid forms of diabetes diabetes) slowly evolving immune-mediated diabetes of adults (LADA) Ketosis prone type 2 diabetes Types of diabetes Other specific types: Monogenic diabetes: Monogenic defects of β-cell function (MODY, PNDM, TNDM, genetic syndromes). Monogenic defects in insulin action; Diseases of the exocrine pancreas; Endocrine disorders; Caused by drugs or chemicals (Drug- or chemical-induced); Infections (Infections); Other uncommon forms of immune-mediated diabetes; Other genetic syndromes are sometimes associated with diabetes. Unclassified diabetes: Temporarily unclassified without a clear diagnosis. Hyperglyacemia first detected during pregnancy: Diabetes in pregnancy, Gestational diabetes.

2. Etiology and pathogenesis
2.1. Type 1 diabetes There are factors: genetic, environmental, immune.
Inheritance Type 1 diabetes is highly associated with frequent elevation of HLA antigens, HLA predominance associated with type 1 diabetes varies by race, HLA B8, B14,15, B18, Cw3, DR3 and DR4 were seen in Caucasian diabetic patients, whereas HLA DR3, DR4 were associated with Asian, African and Latin American type 1 diabetes. HLA DR3 or DR4 was found in 95% of type 1 diabetes compared with 45-50% of Caucasian controls.
Environmental factors Type 1 diabetes can be the result of infection, toxicity that damages the pancreas, and the immune system attacks and destroys pancreatic beta cells. Environmental factors associated with impaired pancreatic islet cell function include viruses (mumps mumps, rubella, coxsackie virus B4), toxic chemicals (nitrogenyl-urea toxic to mice), and cytotoxic toxins. other cells such as hydrogen cyanide from spoiled tapioca or from cassava roots.
Immune factor Humoral immunity:
Circulating antibodies against pancreatic islet cells are found in the majority of patients with type 1 diabetes at diagnosis (60 - 90%) and then decline. In addition, >60% of anti-insulin antibodies were found prior to insulin therapy (autoantibody to insuline: IAA). There are also anti-Tyrosine phosphatase antibodies IA-2 and IA2. Most anti-islet antibodies are directed against Glutamic Acid Decarboxylase (GAD or GADA), an enzyme that localizes in pancreatic beta cells.

Cellular immunity:
Also plays a role in the pathogenesis of type 1 diabetes: it has been studied in BB mice and thanks to monoclonal antibodies, it has been shown that lymphocytic disorders are associated with type 1 diabetes (decreased inhibitory T lymphocytes, and increased T helper/suppressor T lymphocyte ratio).
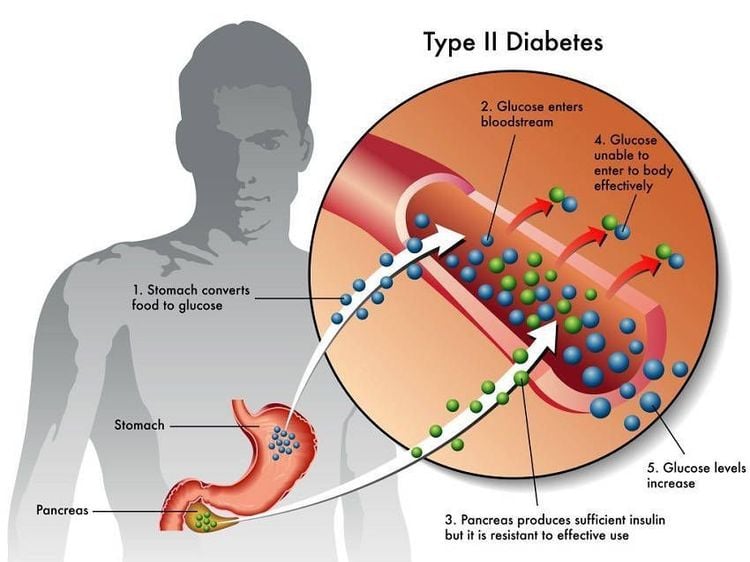
2.2. Type 2 diabetes Genetic factors Dominant inheritance is suggested after studies in identical twins, if one has diabetes then 100% of the other will also have diabetes.
Environmental factors Age, obesity, lack of exercise are risk factors for diabetes. In addition, type 2 diabetes often occurs in different high-risk populations, including insulin resistance, increased adipose tissue abnormalities, increased VLDL, such as increased fasting and postprandial insulin, and elevated blood pressure (in the association). metabolic syndrome).
Insulin resistance in type 2 diabetes is the result of many different pathogenesis. Most of this mechanism is probably the result of metabolic disorders such as hyperglycemia, increased non-esterified fatty acids. On the other hand, recent studies in the pre-diabetic population have found that insulin resistance in muscle tissue occurs very early in the development of the disease. β-cell dysfunction in type 2 diabetes:
Disorders of insulin secretion: Decreased insulin response to glucose: premature phase loss. Rhythmic insulin secretion disorders: slow oscillating phase disturbances. Physiological insulin secretion consists of two types of oscillations: fast oscillations (every 8-15 min, unrelated to glucose), slow oscillations (every 80-120 min, closely related to glucose concentration). Abnormalities of pro insulin metabolism: in type 2 diabetes, pro insulin and intermediate metabolic products/insulin: increased. Decrease in β-cell mass. The role of amyloid (amylin) deposition in pancreatic islets. Found in 90% of cases of type 2 diabetes. Early occurrence causes a gradual loss of pancreatic islet cell mass, especially β-cells.
2.3. Mixed forms of diabetes Slow-onset immune-mediated diabetes of adults (LADA):
The reason for using the word "latent" is to distinguish these delayed-onset cases from typical adult type 1 diabetes. However, LADA does not require insulin therapy at diagnosis. It is initially controlled with lifestyle modifications and oral medications, but progress will require insulin more rapidly than in people with typical type 2 diabetes.
Three criteria are commonly used in diagnosis:
Presence of at least 1 of 4 autoantibodies: ICA, GAD65, IA-2, IAA; Age over 35 years at diagnosis; No insulin therapy is required for 6-12 months after diagnosis. The question of whether slowly progressive immune-mediated diabetes is a distinct clinical subtype or merely a stage in the process leading to type 1 diabetes has caused considerable discussion. . Relative differences between slowly progressive immune diabetes and type 1 diabetes include obesity, features of the metabolic syndrome, better maintenance of pancreatic cell function, and expression of an autoantibody. (especially GAD65) and carry transcription factor 7-like 2 (TCF7L2)).
Ketogenic type 2 diabetes
Over 15 years ago, a form of diabetes prone to ketosis was first described in young African Americans in Flatbush, New York, USA, as a variant of type 2 diabetes. This phenotype has subsequently been reported in populations in sub-Saharan Africa but is least common in populations of European descent.
Usually, these patients are prone to ketosis, which is seen as evidence of severe insulin deficiency, which then goes into remission and does not require insulin therapy. Reports show that subsequent ketotic episodes occur in 90% of these individuals within 10 years, after which the pancreatic beta cells' ability to secrete insulin begins to significantly recover.
The pathogenesis is unclear and no genetic or immunological evidence has been found. It is recommended to consider the possibility of type 2 diabetes mellitus predisposing to ketosis in adult diabetic patients of all ethnicities (except the Caucasian population) presenting with ketosis, but having most of the following characteristics. features of type 2 diabetes. However, the diagnosis can only be established over time.
2.4. Other Specific Types of Diabetes: Juvenile-onset diabetes, known as MODY (Maturity Onset-Diabetes of the Young), was first described by Fajan in 2008. 1960. Later also Fajan and Tattersall further distinguish two different groups of the genre. The common feature of this type of disease is a decrease in the insulin secretion of beta cells, but each type of MODY has impaired regulatory functions differently.
Clinical features of MODY:
+ Early onset disease before age 25;
+ Blood glucose elevation is usually mild;
+ Inheritance by autosomal dominant;
+ No need for insulin intervention for 5 years (or more), from the time the disease is detected.
Cell function gene defects Including young-onset diabetes mellitus (MODY), permanent neonatal diabetes mellitus (PNDM), transient neonatal diabetes mellitus (TNDM) and hereditary insulin deficiency disease syndrome Diabetes is associated with specific clinical features.
These diseases have different phenotypes and response to treatment. GCK MODY leads to mild lifelong hyperglycemia, which declines very little with age. These individuals rarely develop microvascular complications and usually do not require pharmacological treatment for hyperglycemia.
HNF1A MODY, the most common form of MODY, leads to progressive and marked hyperglycemia with a high risk of microvascular and macrovascular complications. These individuals are very sensitive to the hypoglycemic effects of sulfonylureas, allowing people with HNF1A who are treated with insulin to be converted to sulphonylureas. People with HNF4A MODY were similar to those with HNF1A MODY except they had marked macrosomia and transient neonatal hypoglycemia.
Single-gene defect in insulin action This is less common than the single-gene defect in pancreatic beta cells. They often present with features of insulin resistance in the absence of obesity, including hypercholesterolemia, acanthosis nigricans, polycystic ovary disease, and virilization. Diabetes develops only when cells are unable to meet the need for insulin.
Mutations in the insulin receptor lead to a wide range of clinical manifestations and degrees of hyperglycemia. Mild mutations produce type A insulin resistance syndrome. Insulin resistance is a feature of a group of lipid storage disorders characterized by lipodystrophy. Familial partial lipodystrophy is a dominant condition characterized by limb dyslipidemia during young adult life, accompanied by hyperlipidemia and insulin-resistant diabetes.
Diseases of the exocrine pancreas Diseases of the exocrine pancreas or damage to the pancreas can all cause diabetes: pancreatitis, trauma, infection, pancreatic cancer, and pancreatectomy. In cystic fibrosis there is both exocrine pancreatic insufficiency and decreased insulin secretion leading to diabetes, but the relationship between these two defects is not clear.
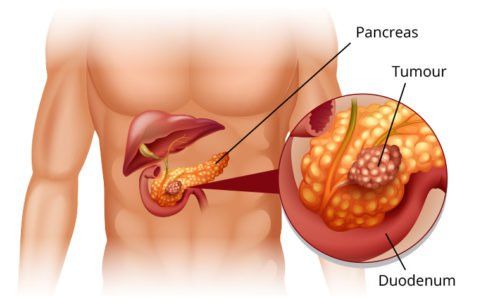
Endocrine disorders Some hormones (growth hormone, cortisol, glucagon, epinephrine) antagonize insulin. Diseases associated with excessive secretion of these hormones are also associated with diabetes mellitus. Somatostatinoma can cause diabetes. Hyperglycemia usually resolves after successful tumor removal.
Drug or chemical diabetes Many drugs can decrease insulin secretion or the effects of insulin These drugs can precipitate. Certain toxins such as pyrinuron (a rat poison) and pentamidine can permanently destroy pancreatic cells.
Some drugs can cause diabetes: Glucocorticoids, Thyroid hormones, Thiazides, Alpha-adrenergic agonists, Beta-adrenergic agonists, Dilantin, Pentamidine, Nicotinic acid, Pyrinuron, Interferon-alpha.
Infection-associated diabetes Viruses in particular are involved in cell destruction and are implicated in causing type 1 diabetes, but their role in its etiology remains uncertain. sure. Diabetes can occur in some people with congenital rubella, Coxsackie B, and viruses such as cytomegalovirus,
adenovirus, and mumps.
Uncommon Forms of Immune-mediated Diabetes Some forms of diabetes are associated with specific immune conditions that have a different pathogenesis or pathogenesis from those that predispose to type diabetes. 1. Insulin receptor autoantibodies can induce diabetes by binding to insulin receptors, thereby reducing the binding of insulin to target tissues. Insulin receptor autoantibodies are occasionally found in patients with systemic lupus erythematosus and autoimmune diseases.
Other genetic syndromes sometimes associated with diabetes Many genetic syndromes are associated with an increased incidence of diabetes, including genetic syndromes associated with severe-onset obesity, including Prader–Willi syndrome, Alstrom syndrome, and many genetically determined subtypes of Bardet-Biedl syndrome.
The second group is the chromosomal abnormalities of Down syndrome, Klinefelter syndrome and Turner syndrome. A final group are neurological disorders, particularly atreia Friedreich, atoria Huntington, and dystonia.

2.5. Unclassified diabetes Diabetes mellitus has become increasingly complex and it is not always possible to categorize all newly diagnosed cases of diabetes into a particular category. They may therefore be provisionally classified into an appropriate category at some point after diagnosis.
The worldwide increase in obesity rates has led to the diagnosis of type 2 diabetes in children and young adults, so the proportion of children and young adults with type 1 diabetes is often overweight or obese. than in the past. In addition, being in ketosis or prone to ketoacidosis is not type 1 diabetes. These problems make the classification of diabetes difficult, especially in diagnosis.
2.6. Hyperglycemia first detected during pregnancy In 2013 WHO updated the definition and diagnostic criteria in 1999 for hyperglycemia first detected during pregnancy. The new classification includes two types of hyperglycemia when first recognized during pregnancy.
One possibility is diabetes, defined by the same criteria as in the nonpregnant. The other possibility is gestational diabetes, as determined by the new recommended glucose cut-off points being lower than those with diabetes.
Currently, Vinmec International General Hospital is providing a Diabetes Screening Package to help patients detect the disease early and improve treatment efficiency.
With this package, patients will receive:
Endocrine CK Exam (by appointment) Oral Tolerance Test (for customers with suspicious fasting blood sugar results) Glucose Measurement HbA1c Measurement Acidity Uric Determination of Cholesterol Determination of HDL-C (High density lipoprotein Cholesterol) Determination of LDL-C (Low density lipoprotein Cholesterol) Determination of Triglycerides Determination of Urea Determination of Creatinine Measurement of AST Activity (GOT) Measurement of ALT Activity (GPT) GGT (Gama Glutamyl Transferase) activity
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.