This is an automatically translated article.
Dermatomyositis is inflammation of the muscles with or without skin lesions. Polymyositis is an autoimmune disease and responds to immunosuppressive drugs. The disease can appear at any age, most often in adolescence (10-15 years old) and middle age (45-60 years old), women are more affected than men. The prevalence of polymyositis in the community is estimated at 5-10 cases/1 million population.
1. Diagnosis of polymyositis
1.1. Confirmative diagnosis Diagnostic criteria of Tanimoto et al. 1995. This criterion has 98.9% sensitivity and 95.2% specificity
Diagnosis of polymyositis is confirmed when at least 4 out of 8 the following symptoms:
myalgia caused by inflammation or pain of a spontaneous nature; Muscle weakness in the proximal extremities; Increased serum CK (creatinine kinase) or aldolase levels; Electromyography has the phenomena of variation of muscle origin: short duration, multiphase motor unit with spontaneous tremors; On muscle biopsy: appearance of skeletal muscle infiltrate with signs of muscle fiber degeneration and necrosis (active phagocytosis, central nucleus or evidence of activity); Arthritis (no erosion on radiographs, no joint destruction) or joint pain; Systemic symptoms: mild fever over 370 C, elevated CRP or elevated erythrocyte sedimentation rate > 20 mm/h using Westergren's method; Anti-Jo-1 antibody positive;

Người bệnh xuất hiện đau cơ
Diagnostic criteria for polymyositis of Bohan and Peter in 1975, including 5 factors:
Muscle weakness in the proximal extremities bilaterally; Muscle biopsy showed symptoms of myositis; Serum muscle enzymes increased; Electromyography with signs of myositis Skin lesions typical of inflammatory myopathy: Gottron rash, red or purple rash in eyelid area, erythema V-shaped on neck and chest, mechanic's hand. Definitive diagnosis of polymyositis
A definitive diagnosis of polymyositis : when all of the first 4 factors are present. Diagnosis is almost certain when polymyositis is present: when the first 3/4 of the factors are present.
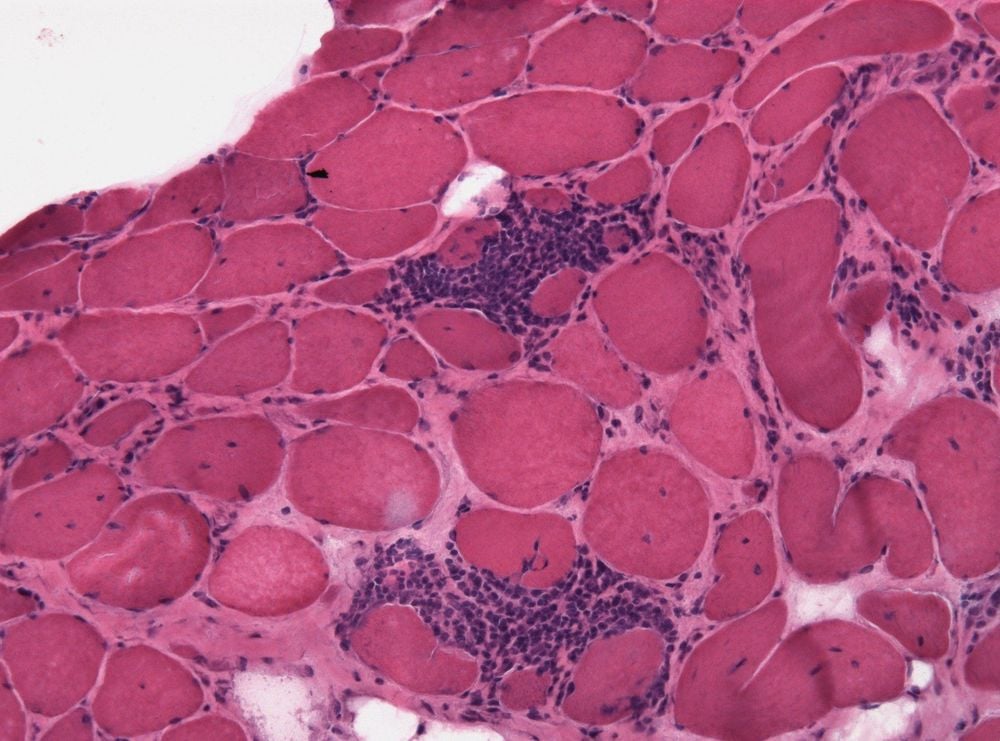
Sinh thiết cơ trên người bệnh viêm cơ
1.2. Differential diagnosis Polymyositis sometimes must be differentiated from other medical conditions that present with muscle weakness:
Chronic or subacute muscle weakness due to neurological diseases: spinal cord injury, fibrosis lateral column chemistry, muscular dystrophy, myasthenia gravis... Neuromotor signs, electromyography and muscle biopsies can help differentiate polymyositis from these conditions. Acute muscle weakness in polymyositis: Guillain-Barré syndrome, transverse myelitis, neurotoxicity, viral myositis. In these conditions, signs of muscle contractures are common, and history, sensory examination, and toxicological and microbiological tests can help in the differential diagnosis. Drug-induced muscle weakness: Thorough examination of the clinical manifestations of polymyositis, especially a history of drug use, can help in the differential diagnosis. Muscle weakness caused by muscle pain, joint pain: In some rheumatic diseases, arthritis can cause muscle weakness. Clinical examination, inflammatory and immunological tests, especially muscle biopsy results, are normal to help differentiate the disease. Muscle weakness in endocrine and metabolic diseases such as hyperthyroidism or hypothyroidism, hyperadrenocorticism. Differential diagnosis of polymyositis is based on endocrinology test results.

Cần chẩn đoán phân biệt với suy tuyến giáp
2. Treatment of polymyositis
2.1. Principles of treatment of polymyositis Drug therapy combined with muscle rehabilitation. Combination of corticosteroids and basic drugs: methotrexate or azathioprine in the common form or cyclophosphamide in the treatment-resistant or interstitial lung lesions. Combined intravenous immunoglobulin infusion is effective but expensive. Prevention of drug-related complications. Survey of associated cancers, especially female genital cancer. 2.2. Treatment with Corticosteroids: is the mainstay of treatment in polymyositis, often in combination with basic treatment drugs (DMARDs).
Oral corticosteroids, with a starting dose of 1-2 mg/kg/day, used once/day or divided into 3-4 times/day if once-daily administration fails to control the disease. Maintain high dose until clinical symptoms of disease are relieved and serum CK enzyme levels fall back to normal levels, about 6-8 weeks on average. Then gradually reduce the dose, the average maintenance dose is 5-10mg/day. High-dose intravenous corticosteroid: 500-1,000 mg intravenously every day for 3 days. Indicated when severe polymyositis, acute progression, cardiovascular damage or severe interstitial pneumonia.

Corticoid đường uống được sử dụng điều trị bệnh
Basic treatment drugs (DMARDs): often combined with corticosteroids in the treatment of polymyositis. This group includes: methotrexate, azathioprine, cyclophosphamide.
Methotrexate
Indications: common forms of polymyositis. Dosage: Oral, 7.5-15 mg weekly, may be increased up to 20 mg weekly depending on patient response. Few undesirable effects (hepatocellular failure, bone marrow failure, pneumonia). Peripheral blood cells and liver enzymes should be monitored monthly when taking the drug for a long time. Azathioprine
Indicated when not responding to treatment with methotrexate. Dosage: Oral administration with a starting dose of 1.5-2mg/kg/day, average dose 150-200mg/day. Reduce dose when clinical symptoms are relieved. Cyclophosphamide
Indicated in cases of resistance to methotrexate or azathioprine) or in the presence of interstitial lung damage. Dosage: once a month intravenous infusion dose of 500mg- 1000mg; for 6 consecutive months; next, can maintain 3 months a dose as above. The drug can be used orally at a dose of 1-2 mg/kg/day, up to a maximum dose of 150 mg/day, but the risk of bladder cancer increases. Undesirable effects: cystitis bleeding, liver cell failure, bone marrow failure, hair loss, feeling hot in the head during infusion.
Thuốc tiêm Cyclophosphamide
2.3. Other measures Intravenous immunoglobulin (IVIG)
Indications: adjuvant treatment in severe polymyositis, unresponsive to conventional regimens. In combination with the above treatments. Dosage: 1-2 g/kg/day, divided into 2-5 days every 4 weeks. Stop the infusion when symptoms of the disease improve. Plasmapheresis (Plasmapheresis)
Indications: adjuvant treatment in severe polymyositis. In combination with the above treatments. Polymyositis causes damage to the skin and muscles for the patient and causes many dangerous complications if not treated promptly. For the treatment process to be highly effective, you should visit the doctor and detect the disease early. To be examined and treated at Vinmec International General Hospital, please register HERE.
MORE:
Infectious myositis: What you need to know Find out information about myositis, polymyositis, dermatomyositis What infection leads to myositis?













