This is an automatically translated article.
Posted by Doctor Nguyen Van Hung, Department of Obstetrics and Gynecology - Vinmec Times City International General HospitalCMV is the most common type of virus causing birth defects accounting for 0.2-2.2% of all live births and is the leading cause of neurological impairment. Approximately 10-15% of children with congenital CMV infection have symptoms at birth and 25% of children suffer long-term effects from CMV infection.
1. Types of CMV infection during pregnancy
CMV infection during pregnancy has 3 forms:
Primary infection (first infection) or Virus reactivation due to previous infection or Re-infection with another strain of virus. The fetus acquires CMV from the mother because the virus can cross the placenta, mainly after primary infection rather than reinfection. If a pregnant mother is infected with CMV during pregnancy, the risk of having a baby with CMV is 30-40%, this rate is only 1-2% if the mother is reinfected.
The risk of congenital CMV infection varies with the time the mother is infected during pregnancy:
0-10% if the mother is infected before pregnancy About 25-30% around the time of conception and in the first trimester 45% during 2nd trimester 47% in 3rd trimester. CMV transmission rates are low in early pregnancy but severity rates are higher with infection during this period. Accordingly, the long-term effects for the baby are also more severe when infected with CMV in the first trimester of pregnancy. The risk of fetal severe symptoms depends on the stage of infection: 70% if infected around the time of conception, 20% in the first trimester, 5% in the second trimester and insignificantly low risk of infection before pregnancy and the third trimester

The majority of CMV infections during pregnancy are asymptomatic. A few symptoms include: fever, fatigue, muscle aches, cervical lymphadenopathy and, less commonly, hepatitis and pneumonia...
Like other herpes viruses, CMV can persist for life in certain locations. It specializes mainly in the salivary glands and can be reactivated at any time, including during pregnancy.
2. Diagnosis of CMV for mother and fetus
2.1 Diagnosis of CMV for infected mother Diagnosis of primary infection in pregnancy:
Presence of CMV IgG antibodies (+) when previously negative or Low affinity IgM (+) and IgG (+) antibodies If not primary infection may not require serological testing For other viruses such as rubella the presence of IgM is often diagnostic of primary or recent infection but not CMV. Cause: IgM CMV can persist for months after primary infection non-specific virus Therefore, to test specific IgG with IgM
To determine the time of CMV infection (before or during pregnancy) it is necessary to test for IgG affinity. If the affinity index is low (<30%) means recent infection (within 3 months) If the affinity index is high (>60%) it means infection for > 3 months or re-infection Diagnosis Non-primary CMV infection is often difficult, and an increase in IgG does not confirm reinfection. In practice, it is only necessary to determine reinfection and transmission to the fetus through CMV-PCR analysis of amniotic fluid.
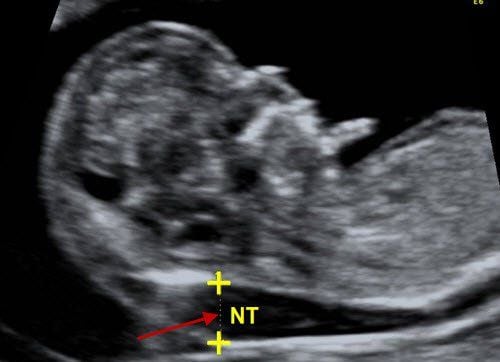
2.2 Diagnosis of CMV in pregnancy Diagnosis of CMV infection requires PCR to look for CMV DNA in amniotic fluid. Amniocentesis is at least 8 weeks after the estimated time of maternal CMV infection and pregnancy >20 weeks.
The most notable false-negative risk factor is the time between infection and amniocentesis <8 weeks and gestational age <18 weeks
3. How is the prognosis and management of CMV-infected fetuses?
Prognosis of poor pregnancy outcomes and outcomes include: timing of CMV infection, fetal abnormalities and CMV infection subtypes. CMV can be classified into 3 groups as follows:
Asymptomatic CMV infection: is the group without abnormalities on ultrasound, normal brain MRI, normal biological indicators, especially normal platelets. This group has a good prognosis in general
Mild or moderate symptomatic group: with isolated biomarker abnormality (on fetal blood test), no brain abnormality on ultrasound or single abnormality on ultrasonography echoes such as thickened intestinal echoes, mild lateral ventricular dilatation, or isolated calcifications. Prognosis in this group is unclear, requiring further follow-up with ultrasound and possibly MRI. Antiviral treatments are still being evaluated, but their application is still being researched. The option to terminate the pregnancy can be discussed
Severe symptom group: g note severe brain abnormalities on ultrasound: microcephaly, enlarged ventricles, white matter abnormalities and cavity formation, intracranial hemorrhage, cortical retardation associated with thrombocytopenia. Prognosis in this group is poor and termination of pregnancy may be advised.

Management of pregnant CMV infection
Since there are no randomized controlled clinical trials, treatment of CMV infection with high-dose valaciclovir should only be used in the study Currently there is no vaccine to prevent CMV Infection Risk reduction strategy infection is changing behavior to reduce direct contact with saliva or urine of young children infected with CMV Prevention of infection by avoiding sharing utensils, eating or drinking together To protect the health of pregnant women and babies throughout During pregnancy, Vinmec International General Hospital provides a package maternity service as a solution to help pregnant women feel secure because of the companionship of the medical team throughout the pregnancy. When choosing Maternity Package, pregnant women can:
The pregnancy process is monitored by a team of highly qualified doctors Regular check-ups, early detection of abnormalities The package pregnancy helps to facilitate convenient for the birthing process Newborns get comprehensive care
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.