This is an automatically translated article.
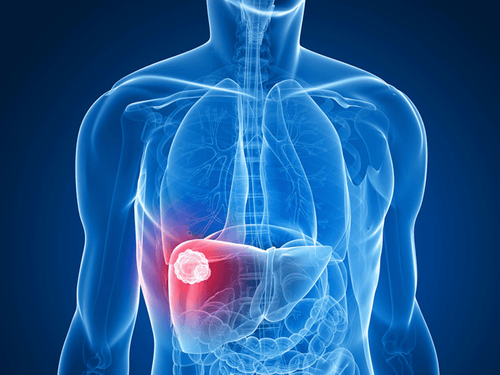
Posted by Resident Doctor, Master Tran Duc Tuan - Department of Diagnostic Imaging - Vinmec Central Park International General HospitalLiver cancer, mainly hepatocellular carcinoma (HCC) is one of the most common cancers in the world. The annual incidence rate is estimated at 500,000-1,000,000 people, the mortality rate is about 600,000 cases globally
In the last 2 decades, treatment for hepatocellular carcinoma (HCC) in the world has been available. These developments have greatly changed the prognosis of this disease.
1. Liver resection surgery
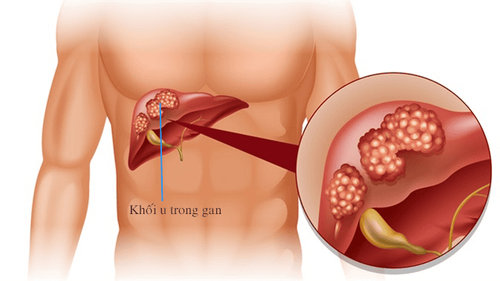
Liver resection is the optimal choice for cases of HCC with indication for surgery, with a good liver function. Thanks to advances in hemostasis techniques and general anesthesia, liver resection is easier and less complicated than in the past. Even for cases of liver tumors larger than 10cm in size, surgery can bring good and safe results. Right-lobe or enlarged left-lobe hepatectomy may also be performed on a cirrhotic background if a good residual liver function reserve is considered. Multifocal liver tumors or vascular invasion of intrahepatic veins are associated with poor postoperative prognosis.For cases where the calculation of residual liver volume is not sufficient for a right lobectomy or an enlarged right lobectomy, right portal vein occlusion is usually performed to cause right lobe atrophy and hypertrophy. left hepatic lobe compensator. In specialized centers for hepatobiliary surgery, hepatectomy for HCC is now quite safe, with a much lower mortality rate than in the past.
Long-term survival outcomes after liver resection have improved significantly, with 5-year survival rates now reaching over 50%. Postoperative recurrence is associated with microscopic metastatic lesions or potentially cancerous nodules in the remaining liver. To date, postoperative adjuvant chemotherapy has had little value in preventing recurrence in clinical trials. Re-surgery or percutaneous destructive methods are still considered options for isolated recurrences. Neoadjuvant therapy before hepatectomy with chemoembolization is not recommended in the international consensus guidelines for the treatment of liver cancer.

2. Liver transplant
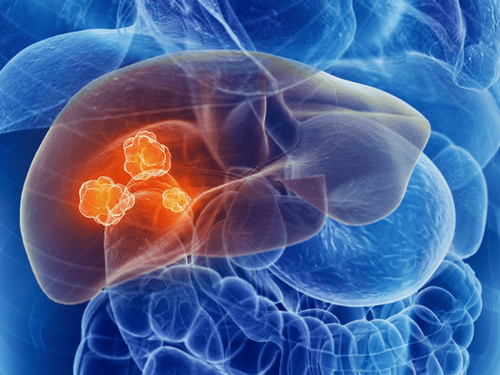
Currently, the widely accepted criteria for indications for liver transplantation are cases of Child C cirrhosis with 1 liver tumor less than 5cm or a maximum of 3 tumors with each tumor size less than 3cm in diameter and no liver cancer. vascular invasion or extrahepatic metastasis (Milan criteria). These cases are often contraindications for hepatectomy because of poor liver function. Some liver transplant centers in the world apply the expanded Milan criteria: 1 solitary tumor less than 6.5cm in diameter or 3 tumors with the largest tumor diameter 4.5cm and the total tumor diameter ≤8cm (UCSF norm). With such selection criteria, the 5-year survival rate reaches 60-75%.Living donor liver transplantation is an advancement in hepatobiliary surgery and organ transplantation. Advances and innovations have been applied in selection, in surgical technique (especially in right hepatectomy) and in post-transplant treatment to achieve maximum safety for liver donors and recipients. In particular, the application of laparoscopic or assisted endoscopic surgery in liver resection from living donors has been initially successfully applied, helping to minimize complications for liver donors. Some technical advances applied in liver transplantation from living donors have brought positive results.

3. Local tumor destruction methods
Local ablation is also a radical treatment for small prostate cancers unsuitable for surgical treatment. Cases of HCC less than 5cm in size and up to 3 tumors are the best indications for local ablation, although some larger tumors can also be treated with this method. this. Local ablation methods are also very useful in cases of liver tumors that recur after surgery, or in cases awaiting liver transplantation for the purpose of controlling tumor progression.Percutaneous ethanol injection therapy (PEIT) is a method of local tumor destruction widely used in the 90s of the last century. However, in recent years, this method has been almost widely replaced by radiofrequency ablation (RFA). Numerous randomized clinical trials have shown that RFA is superior to PEIT in tumor control and survival. This technique also requires less intervention. The engineering-related mortality rate is just under 1%. This technique can be performed percutaneously, during open or laparoscopic surgery, under direct guidance of ultrasound or computed tomography. Cases of liver tumors less than 3cm in size in the periphery are the best choice for RFA.
Combining local destructive treatment with arterial and systemic treatments (multimodalities) is also a trend that is being widely applied. Many studies at home and abroad show that PEIT or RFA combined with embolization gives better results in terms of tumor control as well as survival time than chemoembolization alone.
High Intensity Focused Ultrasound (HIFU) is a completely new non-invasive local ablation treatment. This method uses high-intensity focused ultrasound to kill cancer cells through a cavitation effect combined with a thermal ablation effect. Many reports have shown that this method achieves tumor destruction comparable to RFA. Because there is no need for a needle to puncture the tumor, complications of bleeding and spreading of cancer cells are avoided as is the risk of RFA or PEIT. This method is also applicable to tumors located near blood vessels or biliary tract, as well as cases larger than 5cm in diameter.
Tumor destruction by microwave (microwave ablation), by cryoablation, or by laser are also local methods of tumor destruction that have been applied with positive initial results.
4. Intra-arterial interventional treatment
Chemical embolization (transarterial chemoembolization - TACE or Transarterial Oily Chemoembolization - TOCE) has long been widely accepted as a primary palliative treatment for cases of HCC are no longer indicated for surgery, with proven effectiveness in clinical trials in many centers around the world in terms of reducing tumor size as well as prolonging patient survival time. when compared with systemic chemotherapy or symptomatic treatment.The general principle of the chemical embolization method in the treatment of HCC is the combination of using cytotoxic chemicals injected directly into the artery feeding the tumor followed by occlusion of the artery feeding the tumor by other agents. circuit occlusion. The occlusive agent slows down and blocks the blood flow to the tumor, causing a lack of blood supply to the cancer cells, and at the same time increases the exposure time of the cancer cells to the chemical agents. At the same time, the lack of blood supply of cancer cells also changes the permeability of cell membranes, leading to an increased ability to penetrate chemicals into cancer cells.

5. Systemic treatment
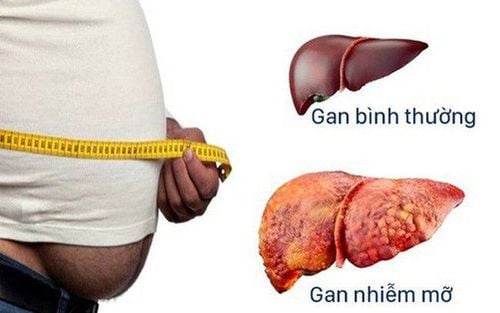
For cases of advanced hepatocellular carcinoma that are not suitable for arterial intervention, so far systemic chemotherapy has yielded limited results while the toxicity is high. due to concomitant cirrhosis in most of these patients.The danger of liver cancer has shown the importance of screening and early detection of the disease. Therefore, Vinmec International General Hospital has provided customers with a package of screening and early detection of liver cancer to screen for liver cancer for people at high risk of diseases such as: alcoholics, cirrhosis, family history of liver cancer, cirrhosis, hepatitis B virus infection, chronic hepatitis C,...
Service selection Package for screening and early detection of liver cancer, patients will be examined, consulted and performed tests, diagnostic imaging to evaluate liver function, liver diseases and liver cancer screening. With a system of modern machinery and a team of highly qualified and experienced doctors, Vinmec is committed to the best protection for the health of patients.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.