This is an automatically translated article.
The article is professionally consulted by Specialist Doctor II Lai Thi Nguyet Hang - Department of Obstetrics and Gynecology - Vinmec Ha Long International General Hospital.
There are many different methods of contraception, but not all methods are 100% effective. The following article provides an overview of the three common types of combined intrauterine contraception, helping couples choose the right method of contraception.
1. Combined hormonal contraceptive method
Birth control pills, the patch, and the ring are combined hormonal methods of contraception. These contraceptives combine the two hormones estrogen and progestin.
These hormonal contraceptives coordinate the release of the hormones estrogen and progestin throughout the body. The hormones primarily prevent ovulation (the release of an egg from one of the ovaries). They also cause a number of changes in the body intended to prevent pregnancy such as thickening of the cervix to prevent sperm penetration as well as thinning of the lining of the uterus.
As with other popular birth control methods, combined hormonal contraceptives are not always 100% accurate. It is estimated that 9 out of 100 women (9%) will get pregnant within the first year of using these methods.

2. What are the benefits of combined hormonal contraception?
Combined hormonal contraceptives have many benefits beyond contraception such as:
Contraceptives can make your periods more regular, have less bleeding, and have a shorter bleeding time. . Reduce menstrual pain. Reduces the risk of cancer of the uterus, ovaries, and colon. Improves acne and reduces unwanted hair growth. These measures can be used in the treatment of certain disorders that cause heavy bleeding and dysmenorrhea, such as fibroids and endometriosis. Continual use of oral contraceptives may reduce the frequency of menstrual migraines (although this is not recommended if the patient with typical migraine has aura (with Aura). It is also used to treat heavy bleeding and pain by stopping menstruation.
3. What are the potential risks of combined hormonal contraception?
Combined hormonal contraceptives are safe for most women, but they always come with a low risk of deep vein thrombosis, heart attack, and stroke. The risk is also increased in women with risk factors, for example, women over the age of 35, those who smoke more than 15 cigarettes a day, or women with multiple cardiovascular disease risk factors such as hyperlipidemia, high blood pressure and diabetes, history of stroke, myocardial infarction, or deep vein thrombosis, including history of typical migraine with aura.
You should not use combined hormonal contraceptives during the first 3 weeks postpartum because the risk of deep vein thrombosis increases in the weeks postpartum. In case you have additional risk factors, you should wait 4-6 weeks from childbirth before using these methods of contraception.
The risk of deep vein thrombosis is also slightly increased in women who use hormonal birth control pills that contain a progestin called drospirenone and in women who use the contraceptive patch. However, the risk of deep vein thrombosis during pregnancy and the weeks after delivery is even higher than taking drospirenone-containing oral contraceptives or using the patch.
4. Can combined hormonal contraceptives be used while breastfeeding?
If you are breastfeeding, estrogen can affect your milk supply. Experts recommend waiting until the 5th week postpartum, when breastfeeding has started.

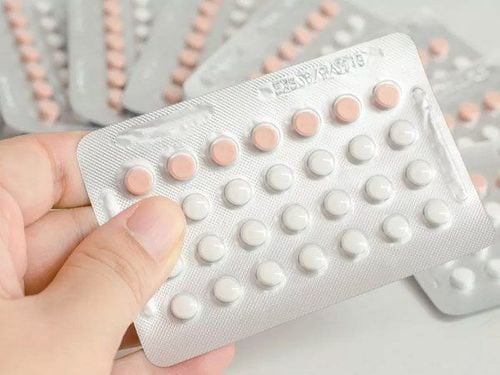
5. Birth control pills
5.1 What types of oral contraceptives are there and how are they used?
21-day cycle pill: Take one pill at a fixed time for 21 days. Wait 7 days before starting a new pack. You will get your period during the week you do not take the pill. 28-day cycle: Take one pill at a fixed time for 28 days. Depending on the brand, the first 21 or 24 pills contain estrogen and progestin. The rest of the pills contain only estrogen, or additional nutrients such as iron but no hormones; or a placebo (with no added hormones or nutrients). You will get your period on the days you take the hormone-free pills. 90-day cycle pill: Take one pill at a fixed time for 84 days. Depending on the manufacturer, the last 7 tablets will either contain no hormones or contain only estrogen. With both types, you will get your period on the last 7 days of every 3 months. 365-day cycle: Take one pill at a fixed time throughout the year. Over time, your periods will become lighter and even stop altogether.
5.2 Side effects when using combined contraception
Possible side effects include:
Headache Nausea Nausea Tension Chest pain Mid-cycle Bleeding Mid-cycle vaginal bleeding is usually a temporary side effect as the body is adjusting to hormonal changes . It will last more than a few months with continuous oral medications.
6. IUD
6.1 What is an IUD?

An IUD is a tiny device that is placed in the uterus to prevent pregnancy. This is a long-term method,
IUD is divided into two types of copper-plated IUD and hormonal IUD. The copper-plated IUD does not contain hormones, it works to prevent pregnancy for up to 12 years. The hormonal IUD uses the hormone progestin to prevent pregnancy. Progestin is a hormone similar to progesterone that the body produces on its own. There are several different types of IUDs on the market such as Mirena for 7 years, Kyleena for 5 years, Liletta for 7 years, Skyla for 3 years.
6.2 How does the IUD work?
Both copper plated IUD and hormonal IUD work by preventing sperm from reaching the egg, of course you can't get pregnant if the sperm doesn't reach the egg.
Copper plated IUD uses copper to prevent pregnancy. Sperm do not like copper very much, so with copper-plated IUD, it is impossible for the sperm to meet the egg.
Besides, the hormones contained in the hormonal IUD prevent pregnancy in 2 ways: by increasing cervical mucus, which helps to lock and trap sperm, these hormones also prevent the egg from leaving the ovary (which is the ovulation), in the end neither egg ever meets the sperm. No eggs, no conception.
One of the great things about IUDs is that they last for years - but they're not permanent. If you decide to get pregnant or you just don't want the IUD anymore, your doctor can remove it quickly and easily. You can get pregnant right after the IUD is removed.
6.3 Can IUDs be used as emergency contraception?
Right! The copper plated IUD is a super good emergency contraception. If you put the IUD within 120 hours (5 days) after having unprotected sex, it's more than 99.9% effective at preventing pregnancy. This method is really the most effective way to avoid pregnancy after sex.
Another great thing about using a copper IUD as emergency contraception: you can keep it and have a really effective birth control that works for up to 12 years.
7 Contraceptive Patches
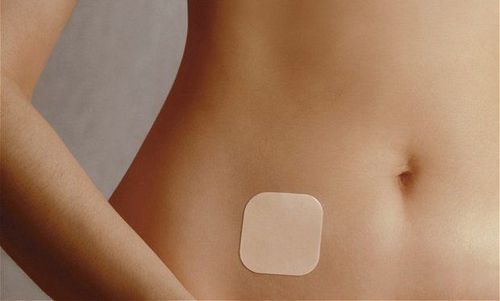
7.1 What is the contraceptive patch?
Small size contraceptive patch (about 4-5 square centimeters) that is stuck on the skin to prevent pregnancy. The patch releases estrogen and progestin, which are absorbed through the skin into the body.
7.2 What should I do if I want to use the contraceptive patch?
You must have a prescription from a doctor, but you can apply and change the patch yourself without going to the doctor. The patch is less effective for women weighing more than 90 kg.
7.3 Instructions for using the contraceptive patch
You can stick the patch on your buttocks, chest (except breasts), upper back, arms or abdomen. You will wear one patch for a week and replace it at the same time in three weeks. The fourth week, you do not wear the patch, at this time, your period will come. After the fourth week, you put on a new patch and so on, the cycle begins. Always wear the patch on the same day of the week, even if you are still menstruating. To use the patch as a long-term contraceptive, wear one continuously each week and do not skip a week.
7.4 Side effects when using the contraceptive patch
Most of the side effects are very mild and go away on their own after a few months of use, they are listed below:Skin irritation Chest tightness Headaches Vaginal bleeding between periods. To choose the right method, you need to have complete knowledge about each method of contraception, go to a reproductive health examination and consult a specialist.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: Acog.org