This is an automatically translated article.
The article was written by MSc Ma Van Tham - Internal Medicine Doctor, Department of Pediatrics - Neonatology - Vinmec Phu Quoc International General Hospital.Congenital pulmonary airway malformation (CPAM), also known as congenital cystic pulmonary malformation (CCAM), is a rare developmental abnormality of the lower respiratory tract. Children with this malformation may present with respiratory failure in infancy or may remain asymptomatic for the rest of life. Many cases are detected early by routine prenatal ultrasound. Surgical resection is a radical treatment.
1. CPAM . classification
CPAM is classified into 5 different types from 0 to 4, some CPAMs are associated with tumor growth in the terminal bronchi. Routine prenatal ultrasonography can increase the rate of diagnosis of CPAM and help better understand the natural course of CPAM.
CPAM can be screened by routine fetal ultrasound and prenatal intervention. The development of modern surgery both before and after birth not only increases the success rate of surgery but also changes the approach and treatment with lesions.
1.1 Epidemiology Congenital airway malformation of the lung is a developmental abnormality of the lower respiratory tract. Although rare, it is the most common congenital lung lesion of the congenital anomalies of the lung. The incidence of congenital pulmonary cysts ranges from 1/8300 to 35,000 live births.
There is no clear association between the incidence and some factors such as maternal age, race. In some cases, lesions present in infancy or infancy with a predominance in boys.
1.2 Pathogenesis 1.2.1 Pathophysiology CPAM is a consequence of anatomical abnormalities of the bronchopulmonary branches. The different types of CPAM differ at different sites in the tracheal tree and at different stages of lung formation. The molecular mechanism of CPAM formation is unclear, but may be due to an imbalance. in cell proliferation and programmed cell death (apoptosis) during organogenesis. Dysregulation of the HOXB5 gene is implicated in this process. This process may be partially regulated mediated by glial-trophic neurotrophic factor (GDNF), a growth factor with Widely affects organ development characteristics through mesothelial-epithelial effects.
GDNF is found in epithelial and endothelial cells from normal fetal lung and in CPAM epithelial cells but not in normal lung of older children (aged 4 months to 3 years). The vascular system is also reduced in CPAM compared with healthy lungs.
1.2.2 Classification of CPAMs are histiocytic lesions consisting of cysts and basal glands arising from tracheal, bronchioles, bronchioles, and alveoli. Large lesions can affect growth due to pressure on adjacent healthy tissues.
CPAM usually communicates with the tracheobronchial tree, although this communication is not usually normal. The arterial and venous drainage from the lesion usually originate from the pulmonary circulation, although vessels connecting to the systemic circulation are often noted.
In the past, the term congenital cystic ductal malformations (CCAMs) was commonly used, which was divided into 3 main categories based on cyst size and cell characteristics (mainly bronchioles, bronchioles or bronchioles - alveoli).
Currently, the term CPAM is commonly used, and there are two additional types (types 0 and 4). Type 0 arises from the trachea and type 4 lesions originate in the alveoli or are of alveolar origin. Each type of CPAM has distinct pathological features.
Type 0 Type 0 is a rare form, accounting for only 1 to 3% of cases, and is derived from tracheal or bronchial tissue. The cysts are small, with a maximum size of 0.5 cm, and are paved by ciliated pseudostratified epithelium. Mucus and cartilage cells are present but the muscle layer is absent. This is a diffuse malformation that forms a mass in the lung. Gas exchange is severely impaired, and affects the risk of infant mortality at birth.
Type 1 Type 1 is the most common form of CPAM, accounting for 60-70%. This type usually originates in the distal or proximal bronchioles of the bronchioles. Because of the clear differentiation of tissue from lesions, this type is almost certainly associated with a late stage of embryonic development (embryos 7 to 10 weeks).
Type 1 lesions consist of clearly thin-walled cysts 2-10 cm in size. These cysts are usually solitary but can also be multi-chambered. They are covered with ciliated pseudostratified epithelium, and the wall is composed of smooth muscle and elastic tissues. Mucus-secreting cells are present in up to one third of cases, and a thin fibromuscular layer may be present below the epithelium.
Islets of abnormal cartilage are found in 5 to 10% of lesions. The adjacent alveoli involved are normal, and in 95% of cases, only one lobe is involved. This type of CPAM has the potential for malignancy, but the magnitude of the risk is not well described.
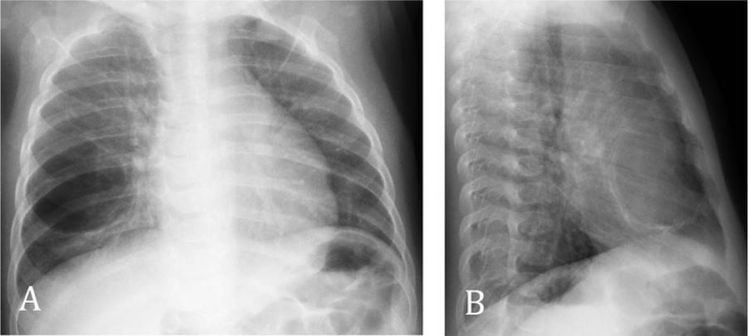
The clinical features of CPAM type 1 depend primarily on the size of the cyst. Large cysts are clearly visible on prenatal ultrasound. If there is pressure on adjacent healthy lung tissue, they can cause neonatal respiratory distress, push the mediastinum to the contralateral side, and flatten the ipsilateral diaphragm. Small cysts can be discovered months to years after birth by chance, or as a focal point of infection.
Type 2 Type 2 lesions account for about 15-20% of CPAM. They consist of multiple cysts 0.5 to 2 cm in size and are a homogeneous mass that fuses with adjacent healthy lung tissue. These cysts resemble dilated terminal bronchi and are lined by columnar epithelium or ciliated mass epithelium.
Type 2 lesions also have thin fibromuscular layers and proliferation of elastic tissues. Mucus and cartilage secreting cells are absent. These masses usually have little effect on the adjacent healthy lung. Isolated lung diseases may have a similar appearance, but unlike CPAM type 2, they have a distinct blood supply system. The combined form of CPAM type 2 and isolated lung has also been described.
Other congenital abnormalities are also observed in CPAM type 2 patients in up to 60% of cases. These malformations include esophageal stricture with tracheoesophageal fistula, bilateral renal aplasia or dysplasia, intestinal stricture, other pulmonary malformations, and other abnormalities of the diaphragm, heart, and nervous system. central and skeletal.
The association with other birth defects suggests that type 2 lesions occur during the third week of pregnancy. In many cases, these associated abnormalities are the first to appear, with CPAM being discovered later. CPAM type 2 has no risk of developing malignancy.
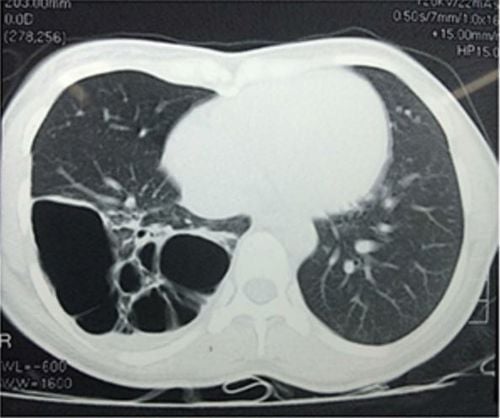
Type 3 CPAM type 3 accounts for about 5-10% of CPAM. They are usually very large, and can affect an entire lobe or several lobes of the lung. They are of alveolar origin and include the proliferative glands of the peripheral airways.
They can be a blend of cysts and solid tissue, or completely solid. Because they are large and undifferentiated, CPAM type 3 is also thought to form early in pregnancy (26 to 28 days of pregnancy). It consists of a large number of follicles less than 0.5 cm in size and is lined by a mass epithelium without cilia. They have thin fibrous layers and increased elastic tissue, similar to type 2 lesions. Mucus and cartilage secreting cells are absent.
Babies with this lesion are usually detected in utero or at birth, often with severe respiratory failure or death in infancy. This type of CPAM was also not associated with malignancy.
Type 4 Type 4 lesions account for 5 to 10% of CPAM. These cysts have a maximum size of 7 cm and are composed of cells lining the alveoli, flattened, without cilia, without any mucus or muscle cells.
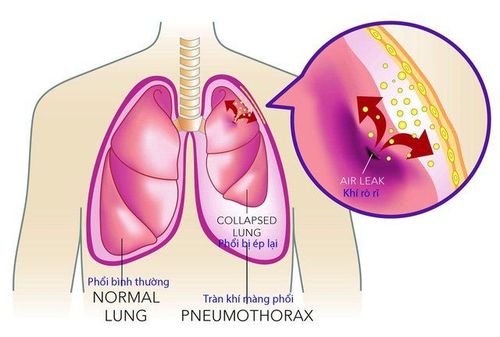
Type 4 CPAM can be present at birth or in childhood, often with tension pneumothorax or infection, but can also be detected incidentally in asymptomatic patients. Most importantly, this CPAM subtype is strongly associated with malignancy, especially with pleural myeloma (PPB).
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.