This is an automatically translated article.
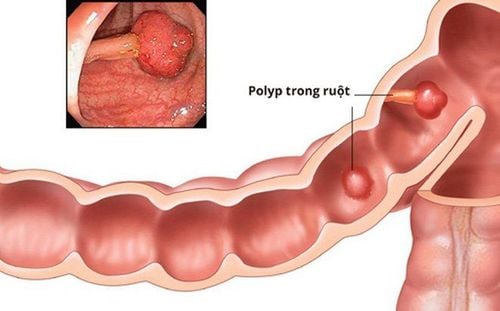
The article is professionally consulted by Master, Doctor Duong Xuan Loc - Gastroenterologist - General Surgery Department - Vinmec Danang International General HospitalFamilial polyposis syndrome (FAP) is an inherited disease, diagnosed when a person has more than 100 polyps in the colon, usually detected in middle age, most commonly by age 35. If FAP is not If detected and treated early, it can progress to colon cancer. There is also an increased risk of developing cancer in other organs, including the stomach, small intestine and pancreas, and bile.
1. Associated symptoms of familial polyposis (FAP)
Not all symptoms in FAP patients are cancer-related. Some accompanying symptoms may include:Benign bone tumors are often found in the jawbone. Extra, missing or undeveloped teeth. Congenital hypertrophy of the retinal pigment epithelium (CHRPE). Benign (noncancerous) skin changes, such as epidermoid cysts and fibroids. Adrenal mass.
2. Classification of familial polyposis
Colonic polyposis is a familial disease, the FAP classification is based on clinical features, including:Classical FAP: Characterized by more than 100 colonic polyps. Colectomy is often the most effective treatment to reduce the risk of colon cancer.
Impaired FAP (AFAP): This form may present from 20 to 100 polyps. People with AFAP often go on to develop multiple colon polyps throughout their lives and have an increased risk of developing colorectal cancer if the polyps are not removed. People with AFAP tend to develop polyps later in life than people with classic FAP; however, this factor can vary from family to family and regular follow-up for early detection is important. It has not been determined whether families with AFAP have the same risk of other cancers as families with classic FAP.

Epithelial cysts - are tumors in or under the skin. Fibroids. Desmoid tumors - are fibrous tumors that can develop anywhere in the body. Osteosarcoma - is a tumor in or on the bone. Turcot syndrome: Considered a variant of FAP syndrome or Lynch syndrome rather than being inherited. People with Turcot syndrome tend to develop multiple colon polyps, an increased risk of colorectal cancer, and an increased risk of brain tumors. The two most common types of brain tumors in Turcot syndrome are:
Glioblastoma: This type of brain tumor is a type of astrocytoma that is common in families with Lynch syndrome. Adenocarcinoma: This type of brain tumor begins in the cerebellum and back of the brain, occurs most often in children, and is often found in families with symptoms of FAP.
3. What causes classical FAP and its subtypes?
FAP is passed down from generation to generation in a family. Mutations (changes) in the APC gene are the cause of FAP, AFAP, Gardner syndrome, and Turcot syndrome, putting a person at increased risk of colorectal or other gastrointestinal cancers.On genetic testing, some individuals with colon polyps were found to carry 2 mutations in the MUTYH gene, also known as the MYH gene, leading to MUTYH-associated polycystic disease (MAP). People with FAP or AFAP may be ordered to have a blood test to look for mutations in the APC or MUTYH gene. If a mutated gene is found, other family members are also at increased risk for FAP or AFAP.

4. How are classical FAP and its subtypes inherited?
Normally, each cell receives two copies of each gene: one inherited from the mother and one inherited from the father. Parents with a genetic mutation can pass on either one copy of the normal gene or one copy of the mutated gene. Therefore, a child with a mutated parent will have a 50% chance of inheriting that mutated gene. The brother, sister or parent of a person with the mutated gene also has a 50% chance of carrying the same mutated gene.Preimplantation genetic diagnosis (PGD) is a procedure performed in conjunction with in vitro fertilization (IVF). It allows people who definitely carry the gene mutation to reduce the likelihood of passing the mutant gene on to their children.
The mother's eggs will be removed and fertilized in a laboratory. When the embryo reaches a certain size, a cell is removed to check for genetic status. The parents can then choose to implant the embryo without the mutation. PGD has been used for more than 2 decades and has been used for a number of syndromes with a genetic predisposition to cancer.
5. Are classic FAP and its subtypes common?
FAP and AFAP are both uncommon. Specific estimates of the number of people with FAP range from 1/22,000 to 1/7,000. About 30% of people with FAP have no family history and are the first in their family to be diagnosed with the condition.Most colorectal cancer is sporadic, which means it occurs randomly and is not related to FAP or other genetic syndromes. Only less than 1% of colorectal cancers are thought to be FAP. Gardner syndrome and Turcot syndrome are both relatively rare.
6. How are classical FAP and its subtypes diagnosed?
Classic FAP is usually diagnosed when a doctor finds multiple polyps in the colon rather than based on lab test results. A person with more than 100 colon polyps will be diagnosed with FAP. AFAP is usually suspected in people with 20 to 100 colon polyps. Gardner syndrome is suspected when a person has multiple colonic polyps and/or colorectal cancer along with several of the benign tumors listed above. Turcot syndrome is suspected when a person has multiple colon polyps and/or colorectal cancer, along with a glioblastoma brain tumor or medulloblastoma. Your doctor will order additional blood tests to help look for mutations in the APC gene and/or the MUTYH gene if a person is suspected to have FAP or its subtypes. If a mutated gene is found, other family members should also get tested to see if they carry the mutated gene, for early detection and timely treatment.
7. What is the cancer risk from classical FAP and its subtypes?
Colorectal cancer: 100% without polyp removal Desmoid tumor: 10% to 20% Small intestine: 4% to 12% Pancreatic cancer: 2% Papillary thyroid cancer: 2% to 25% hepatoblastoma: 1.5% Brain or lower central nervous system tumor: 1% Stomach cancer: 0.5% Small bile duct cancer Small adrenal cancer
8. What are the classical FAP screening methods and its subtypes?
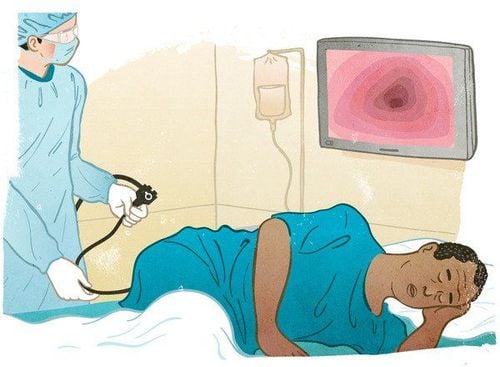
Sigmoidoscopy or colonoscopy: Every 1 to 2 years, starting at age 10 to 11 for people at risk for FAP. Endoscopy begins at age 18 to 20 for people at risk for AFAP. Annual colonoscopy: If polyps are found until resection of the rectum is indicated. Surgery: There are different types of colon surgery for people with FAP and AFAP. People with classic FAP may require a total colectomy, due to the high number of polyps and the high risk of colorectal cancer. This is a major surgery and may involve small bowel surgery. After colon surgery, doctors will monitor patients with sigmoidoscopy at regular intervals, depending on the type of surgery. Usually patients will have a colonoscopy at 6 to 12 months if there is still some rectal tissue or 1 to 4 years if all the rectal tissue has been removed and a small bowel pouch is present. Upper Colonoscopy (EGD): At age 25 to 30, or once colorectal polyps are found, whichever occurs first. This test is to check for duodenal polyps. Duodenal polyps increase the risk of duodenal cancer if not removed. Annual thyroid ultrasound: It is recommended to start at age 25 - 30. Computed tomography (CT) or magnetic resonance imaging (MRI): May be ordered if a person has a personal or family history of desmoid tumors. Screening options for Gardner syndrome are considered similar to those for classical FAP, with the addition of regular skin examination by a dermatologist. Screening options for Turcot syndrome are considered similar to those for Lynch syndrome or FAP, but with additional brain tumor screening.

9. Measures to reduce cancer risk?
The risk of cancer in FAP and AFAP can be reduced through removal of colorectal and duodenal polyps. Many studies are underway to find out if taking the drug can be effective in reducing the risk of cancer.A recent clinical trial showed that a combination of 2 drugs, sulindac (Clinoril) and erlotinib (Tarceva), reduced the number of colorectal and duodenal polyps. However, this result has not yet been incorporated into the treatment strategy and needs to be studied further.
10. What questions should be asked when booking a consultation from a doctor?
If you are concerned about your risk of colorectal cancer or other types of cancer, you should discuss it with a qualified doctor. Consider asking the following questions:What is the risk of developing colorectal cancer? How many colon polyps do I have in total? What type of colon polyp did I have? What is the risk of developing another type of cancer? What can I do to reduce my risk of cancer? What are the measures for cancer screening and prevention? Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit. and hospital treatment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.