This is an automatically translated article.
The article was written by Specialist Doctor II Tran Van Trong - Specialist in Pediatric Surgery, Plastic and Aesthetic Surgery, Vinmec Danang International General Hospital.These diseases in children often appear quite common and will disappear in adulthood. But in some cases, there are signs of swelling, redness, and serious infection. Early recognition of signs of pathology in infants will help parents have a more timely treatment plan.
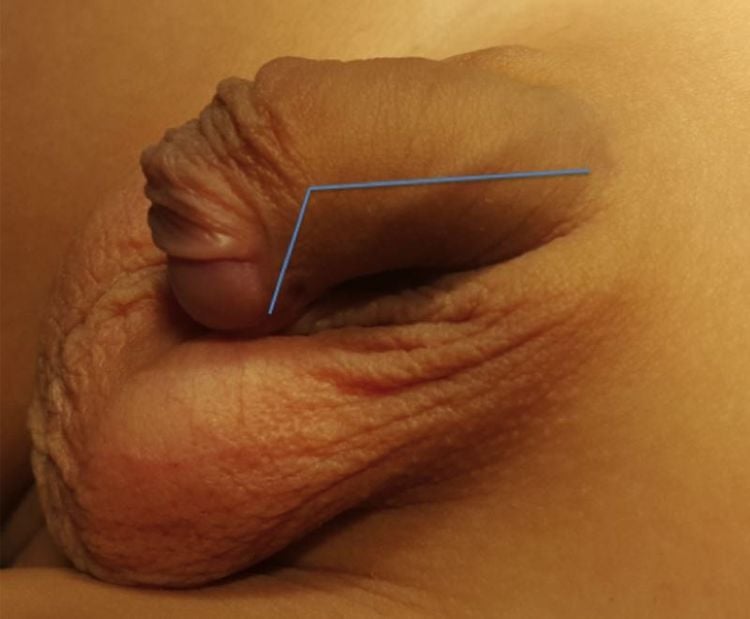
1. Narrowing of the foreskin
Basic understanding of foreskin stenosis:
Mostly physiological in boys after birth: about 96% in newborn, by 1 year old, remaining 50%, 3 years old remaining 10%. By the age of 16, this rate drops to 1%. The foreskin narrowing: the foreskin is narrow and cannot be pulled upside down to reveal the glans.

Within the first three years of life, with a child's physiological erection, the foreskin is usually dilated enough to be able to roll back without any problems or pain. Parents should not try too hard to reverse the foreskin. This can be painful for the baby and damage the foreskin, causing narrowing of the foreskin later on. Simply clean, wash the penis from the outside using warm water and neutral soap (bath soap). If the foreskin is not wide enough to expose the glans, conservative treatment is by applying steroid cream to the foreskin twice a day for 4 to 8 weeks. After 2 weeks, parents can pull back the foreskin very gently to gradually widen the foreskin. You can practice 2 times a day, 20 times each time. Take care not to damage the skin. If the foreskin is exposed, cream can also be applied to the part of the glans that is exposed. The foreskin is then returned to its normal position. This treatment is successful in most children. But it usually has to be repeated over a period of time (more than 1 year is recommended) for a longer lasting effect. Surgery should be performed when narrow foreskin causes recurrent local infections, has failed conservative treatment, and the child is at risk of strangulation (partial stenosis).
First aid when strangling the foreskin.
2. Low deviated urethral malformation
2.1 What is a low urinary hole? A low urinary opening (low opening of the urethra) is a urinary opening that is located low compared to its normal position at the top of the glans. The position of the urethral opening is far from the top of the glans, the more severe the disease, the more difficult the surgery.
Low urinary opening is a common malformation in boys (incidence 1:300).
2.2. Manifestations of low urinary opening The urinary hole is located low compared to the normal position at the top of the glans. The low urinary opening makes the child when urinating, the urine stream is not straight forward, but often deviated to the bottom of the leg or to the back.



Low urinary opening or accompanied by some diseases also in the genitals such as undescended testicles, inguinal hernia. In addition, severe low urinary tract (urinary opening is located near the scrotum) may be accompanied by anomalies of the penis lying low compared to the scrotum (scrotal penile transposition), scrotum bisecting. In some cases this is also a manifestation of disorders of sexual development (intersex).

2.3 How is low urinary tract affected? Low urinary tract disease does not cause difficulty urinating, but the urinary tract (urethra) may be poorly developed. When the urinary hole is low, boys have to urinate like women. Therefore, the degree of influence is severe or mild based on the location of the urinary opening.
For penile curvature, if not treated, later in adulthood, causing difficulties in intercourse. Severe cases of curvature require multiple surgeries to correct.
In the lower urinary tract, abnormal orifice position combined with penile curvature can lead to infertility later in life.
2.4 Suitable age for correction of low urinary tract malformation The most suitable age for surgery is from 6 months old to before 18 months. Surgery should be performed before 18 months of age because the child when he grows up will not remember what happened before this age, thus avoiding guilt for the boy later. According to the statistical results of many studies, this age of surgery also has a better success rate than late surgery. For special cases such as small penis, boys are operated later. The decision of the time of surgery in these cases is up to the specialist.
2.5 How is corrective surgery performed? Surgery to treat the low urinary hole is necessary to bring the urethra back to the position at the top of the glans and create a straight shape for the penis, helping the boy not to feel guilty when he grows up and most importantly if the urethra is at the top of the penis. If the position is normal, the probability of having children is higher when getting married later.
Surgical methods to treat the disease are performed depending on the severity of the malformation. In the majority of cases, only corrective surgery is needed in one visit. Severe cases require 2 surgeries.
Low urinary opening surgery is difficult plastic surgery, so complications such as fistula, urethral stricture (urinary tract), urethral diverticulum... after surgery. Urethral fistula is the most common (10 - 30%). When a fistula occurs, it is necessary to wait 6 months after surgery to repair the fistula.
Length of hospital stay: depending on whether the disease is mild or severe, the hospital stay is long or short, mild form 5-7 days, severe form 12-14 days.
Children need to be periodically re-examined according to the doctor's appointment, the time of re-examination depends on the disease, the surgical method of each specific case.
3. Inguinal hernia, hydrocele, spermatic cord cyst
Children's inguinal hernia, spermatic cord cyst or hydrocele are different disease manifestations of the same condition "with peritoneal duct". All three diseases share the same pathogenesis, etiology, but the epidemiology, incidence, and risks are different.
Hydrocele or hydrocele is a condition in which water appears in the peritoneal canal causing the inguinal scrotum to swell.
Currently, the mechanism of incomplete closure of the peritoneal canal is explained in different ways and remains unclear.
The greatest risk is incarcerated inguinal hernia, leading to intestinal necrosis and perforation, peritonitis, sepsis, which can be life-threatening, especially in children. A strangulated inguinal hernia is considered an emergency. With timely surgical release, perfusion will be restored, the bowel will return to normal, without having to remove the necrotic bowel. Therefore, families who discover that a child has symptoms of constant pain in the inguinal region should be prevented from strangulated inguinal hernia and taken immediately to an emergency facility.
In boys, the pressure in the spermatic cord caused by a strangulated hernia capsule also reduces blood flow to the testicles.
In girls, the ovary or fallopian tube can descend into the hernia capsule and become blocked here. Ovarian obstruction is also an emergency, causing pain in the groin area and lack of blood supply to the ovaries. However, it does not cause dangerous infections such as gangrene and perforation of the intestine.
The incidence of inguinal hernia is about 10-20 cases per 1000 full-term infants, preterm infants are more susceptible. Right side is more common than left side, about 10% is bilateral.
Inguinal hernia is 6 times more common in boys than in girls. In girls, obstruction of the ovaries and fallopian tubes is more common than bowel obstruction. Therefore, the overall rate of intestinal obstruction is higher in boys than in girls.
The rate of detection of peritoneal tubules decreases with age. In neonates, 80-90% of babies are born with a peritoneal tubule. Inguinal hernia is 20 times more common in premature infants weighing less than 1500g compared with term infants. At autopsy, it is found that about 30% of adults still have peritoneal tubules. The reason why only a few peritoneal tubules develop into inguinal hernias or hydroceles, spermatic cord cysts is still not well understood.
How to recognize: Inguinal scrotum is larger than normal, disproportionate, may or may not be painful, changes in volume when lying down, when abdominal pressure is increased (straining, crying, running,...).
Timing of surgery: Hydrocele and spermatic cord cyst: after 1 year of age. Inguinal hernia: Surgery as soon as possible to prevent the risk of intestinal strangulation, for girls, the sooner it is necessary to operate because if the hernia is a tube or ovary, it is easy to suffocate because there is no peristalsis.
Re-examination after 1 week, 1 month, 3 months, 6 months and 12 months after surgery.
4. An undescended testicle (testicle not palpable)
4.1. What is an undescended testicle? The testicle was not palpable in its normal position (scrotum).
Is the most common congenital anomaly of the genitourinary system in children. Understanding the movement of testicles as well as complications of undescended testicles will help young parents make the right decisions when treating.
Along with the development of the fetus, the testicles move from the abdomen to the scrotum at the time just before birth. But for some reason, this process is affected, leading to the condition that the child is born with an undescended testicle, or more precisely, a testicle that has not yet descended into the scrotum.

Undescended testicle is the most common congenital anomaly of the pediatric genitourinary system, occurring in 30% of preterm boys and about 4% of term infants.
Within 6 months after giving birth, the testicles can continue to move and descend to the correct position in the scrotum. However, only half of testes with undescended testicles are able to move on their own during this period. If after 6 months the testicle is not in its proper place, the child needs to be treated.
Otherwise, the growth of the testicles will be limited, in the long run may affect fertility, even testicles may become malignant.
4.2 Diagnosis Parents often find that their baby's scrotum is uneven. If in doubt, you should immediately go to a pediatric surgical facility for examination. It should be noted that 70% of testes that are not in the scrotum can be palpated by the paediatrician simply by physical examination. In the remaining 30%, the location of the testicle cannot be determined, it may be present – very deep, even intra-abdominal, or may not be present at all. - Another case of pathology, that is when the testicles are palpable in the scrotum, sometimes they are not palpable. This is called a "spring testicle", the testicle moves up and down between the scrotum and the groin. Usually, "spring testicles" do not need to be treated, but need to be examined and monitored regularly because as the child grows, the elasticity of the "spring" does not develop, leading to true undescended testicles. the.
4.3. Treatment If the child's testicles cannot be palpated in the scrotum after 6 months, it is necessary to take the child to a pediatric surgical facility for examination and treatment. The most basic and effective treatment is surgery to lower the testicle into the scrotum.
4.4. Why surgery is necessary, for the following reasons:
High body temperature can limit testicular growth, affect testicular spermatogenesis, can cause infertility in the future. Testicles that are not in their correct position have a much higher risk of malignancy than normal testicles. High testicles are susceptible to trauma or testicular torsion. Asymmetrical bilateral scrotum affects affect the psychology of children Sometimes inguinal hernia occurs because the testicles do not move, the inguinal hole is not closed.
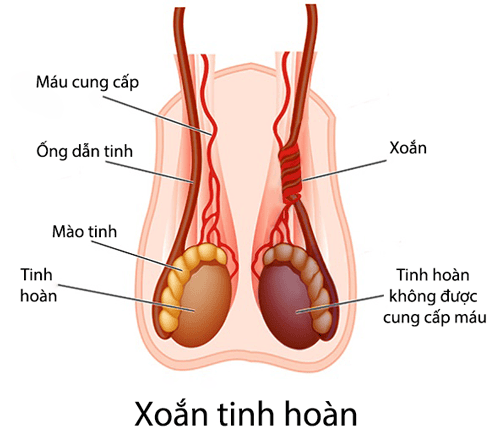

4.5. Prognosis Studies have shown that undescended testicles have almost no effect on fertility or male hormones. However, despite the surgery, the patient still needs to be monitored and periodically re-examined by the pediatric surgeon.
5. Umbilical hernia
5.1 What is an umbilical hernia? A hernia occurs when an organ or part of an organ protrudes out of its normal position in the body. Umbilical hernia occurs when internal organs in the abdomen bulge out, forming a protrusion in the navel area. The hernia may contain fluid, an internal organ such as the intestine, or other organs from the abdomen.
Experience placing coins. However, scientific studies show that this method is not effective.
Umbilical hernias occur most often in babies born prematurely or with low birth weight. This defect occurs more often in girls.
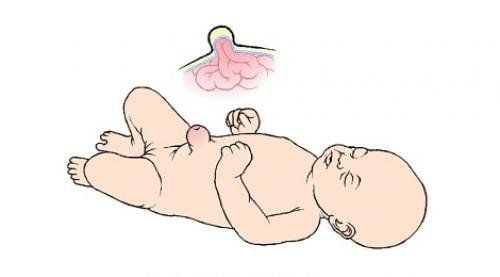
5.2 Why does the baby get an umbilical hernia? Babies are born with the umbilical cord attached to the abdomen. The umbilical cord enters the body through a small opening in the abdominal wall muscle and is cut after the baby is born.
Within 1-2 weeks after birth, the umbilical cord gradually atrophies and falls off, the wound heals and forms the baby's navel.
The hole in the abdominal wall where the umbilical cord passes will close on its own. An umbilical hernia occurs when the abdominal muscles do not close properly.
5.3 When is an umbilical hernia usually discovered? When your baby cries, coughs, stretches to have a bowel movement or when he sits up. This mass may get smaller or disappear as your baby relaxes. Umbilical hernias are usually painless.
Complications Umbilical hernias in young children rarely cause complications. However, sometimes a loop of bowel can get stuck in the hernia sac and cannot be pushed back into the abdomen, which will cause pain in the umbilical region and damage the intestinal tissue, severe can lead to bowel necrosis, disseminated infection. in the abdomen, life-threatening.

How is umbilical hernia treated? Most cases will go away on their own by the time the baby is 1 year old. As the baby grows, the abdominal muscles get stronger and can close the hole in the abdominal wall, the hernia will go away on its own (usually by the time the baby turns 1 year old). In some cases, hernias disappear after 4-5 years of age.
Surgery is usually indicated for cases where the hernia is very large and causes pain, or:
Threatening strangulation or strangulation Enlarged when the baby is 1 or 2 years old. Does not disappear when the baby turns 4. During surgery, the doctor will make a small incision at the base of the navel. The herniated organization was brought back into the abdomen, the opening in the abdominal wall was closed.
Prevention: There is no way to prevent an umbilical hernia, except trying to avoid premature birth.
6. Acute intussusception
Intussusception is a pathological condition in which the upper intestine enters the lumen of the lower intestine causing mechanical obstruction of the gastrointestinal tract.
Intussusception is a common pediatric emergency and the leading cause of intestinal obstruction in young children. Intussusception in breastfed infants is mostly acute, with rapid bowel necrosis. Intussusception in children is mostly subacute and chronic.

In older children, the causes are often mechanical: Meckel's pouch, polyps in the intestinal lumen, various malignancies, intraluminal hemangiomas, double bowel, ectopic pancreatic nodules. One of the possible pathological conditions is lymphoma that manifests in the intestinal wall. Intussusception in young children is usually spontaneous intussusception, with unknown cause, accounting for 75-90%. Some theories put forward are:
Neuro-humoral causes: in breastfed babies, due to the dominant activity of the X nerve (tenth nerve) causing increased intestinal motility, leading to intussusception. Due to viruses and bacteria: when the body is infected, inflammatory nodes develop, the cecum is edematous, increased intestinal motility easily leads to intussusception. Anatomical factors: In children under 4 months of age, the size of the ileum and the cecum is not significantly different, from the 4th to the 12th month, the cecum grows faster than the ileum and there is a difference in peristalsis. create favorable conditions for the common type of intussusception is ileocecal intussusception. Intussusception causes damage depending on the nature and time since appearance
Gastrointestinal obstruction: causes painful symptoms Abdominal cramps, vomiting, abdominal distention, bowel obstruction, stagnation of circulation to and from the intussusception: causing blood stasis, bleeding into the intestinal lumen, causing bloody bloody stools. necrosis of the intussusception segment Diagnostic signs:
Abdominal pain: sudden, severe, crying out intermittently, the time between attacks lasts from 15 to 30 minutes, the attacks gradually. Vomiting: occurs with pain, vomiting milk or new food. If vomiting yellow fluid means the time of onset is long. Blood in the stool: small amount, about 10 hours after the first symptom of abdominal pain. Early signs of bloody diarrhea are common in young children. If the bowel is bloody less than 5 hours early and has a lot of blood, the intussusception is often tight and the prognosis is severe. Abdominal examination: due to the child's pain, it is difficult to feel the cage mass. To find the intussusception, examine gently with the patient lying still and out of pain. If the abdomen is distended and painful, late intussusception has complications. Rectal examination: there may be blood in the hand, the rectal balloon is hollow, the tip of the intussusception may be palpable. Patients arriving late have signs of water-electrolyte disturbances, or in a state of shock Systemic signs: in case of late arrival, patients have signs of water-electrolyte disturbances, or in a state of shock. In older children: presenting subacute or chronic intussusception
Abdominal pain: usually the main presenting symptom, pain lasts intermittently, pain is less frequent, few pain per day, still passing or defecating . Maybe a few episodes over a long period of time. Vomiting or nausea: occurs with pain. Blood in stools: less common in older children Cage: more palpable than in young children General: fatigue, poor appetite, possibly thin. Patients arriving late with signs of electrolyte disturbances, or in shock
Treatment:
Air intubation: Inflating through the anus, colon, small intestine Manual intubation Laparoscopic removal surgery Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical professionals, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Sean Primley and Duncan Wilcox. Hypospadias . Operative pediatric surgery. Edited by McGraw-Hill. Mosby 2014, pp. 790-799 Low urinary tract. Pediatric treatment protocol. Children's Hospital 1. Medicine Publishing House, 2013, p. 1140-1145 SEE ALSO:
How does surgery for foreskin narrowing take place? Children's inguinal hernia: Causes, symptoms, diagnosis and treatment Intussusception: Causes, symptoms, diagnosis and treatment














