This is an automatically translated article.
Article by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
Graft-host disease in kidney transplant recipients is extremely rare. The pathogenesis of graft-host disease is not fully understood, but it may be triggered by destruction of host tissues through a number of different mechanisms involving cytotoxic T cells. donation cells.
1. Overview
Kidney transplantation is considered the gold standard treatment in patients with end-stage renal disease. This method significantly improves the quality and survival of patients compared to dialysis. Although much progress has been made over the years, the management of patients during post-transplant follow-up remains clinically challenging. The success of a kidney transplant is related to the prevention of acute rejection. Immunosuppressive therapy is evaluated to be able to significantly improve outcomes, reduce rejection rates after kidney transplantation.
However, chronic immunosuppression can increase the risk of various diseases, including chronic systemic kidney disease, infection, and post-transplant cancer. In addition, kidney transplant recipients are at increased risk for gas gastrointestinal complications, which are a major cause of morbidity and mortality after transplantation.
2. Gastrointestinal complications in kidney transplant recipients
Gastrointestinal complications in kidney transplant recipients may result from typical infections, such as cytomegalovirus (CMV) infection and immunosuppression-mediated damage to the gastrointestinal mucosa .
Post-transplant inflammatory bowel disease (IBD) can arise from an inappropriate immune response to intestinal antigens. Immunosuppressive therapy could theoretically combat this inflammatory process. However, it may allow dysregulation of the intestinal immune system, ultimately leading to the development of post-transplant IBD. Kidney transplant recipients can develop a new-onset form of IBD despite being immunosuppressed.
3. Inflammatory bowel diseases in transplant patients
Inflammatory bowel diseases in transplant patients are mostly colitis and are characterized by similar symptoms but different pathophysiological features. A variety of clinical conditions have been described, including the following: Table 1: Clinical and histological features of inflammatory bowel diseases in renal transplantation.
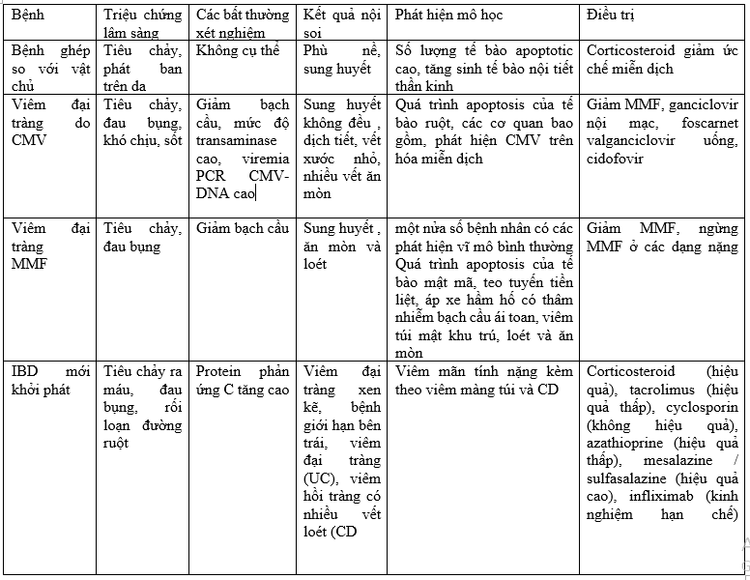
CMV: Cytomegalovirus; PCR: Polymerase chain reaction; DNA: Deoxyribonucleic acid; MMF: Mycophenolate mofetil; IBD: Inflammatory bowel disease; UC: Ulcerative colitis; CD: Crohn's disease. Several studies report that the incidence of IBD in solid organ transplantation is approximately 10 times higher than that observed in the general population, especially in liver transplant recipients, the occurrence of IBD in renal transplantation. rarely reported. The aim of this review was to evaluate the natural history of inflammatory bowel disease in kidney transplant recipients, with particular emphasis on morbidity, clinical features, and potential therapeutic efficacy. Furthermore, a brief overview of the outcomes of kidney transplantation in patients with pre-existing inflammatory bowel disease was also reported.
4. Clinical features of graft disease - gastrointestinal host after kidney transplantation
The term GVHD (graft-versus-host disease) refers to a clinical syndrome that occurs in transplant patients with damage to target organs such as the skin, liver, gastrointestinal tract and, rarely, muscles other officials. It is more common in bone marrow transplants and rarely occurs in solid organ transplant recipients. The incidence is higher in small bowel transplant recipients (5%), while in liver transplant recipients it occurs 1 to 11 weeks after transplantation, with frequency ranging from 0.1% to 1 % and mortality exceeds 75%.
Graft-host disease in kidney transplant recipients is extremely rare, with only 6 cases reported in a recent review by Guo et al. Clinical manifestations include diarrhea (in cases involving the gastrointestinal tract), skin rashes (in cases involving the skin), and impaired renal function. The prognosis of GVHD after renal transplantation is generally better than that of GVHD after other solid organ transplantation, possibly due to fewer donor-derived lymphocytes in renal transplantation compared with other solid organ transplantation. Only 2 out of 6 patients died of GVHD in the renal transplant setting.
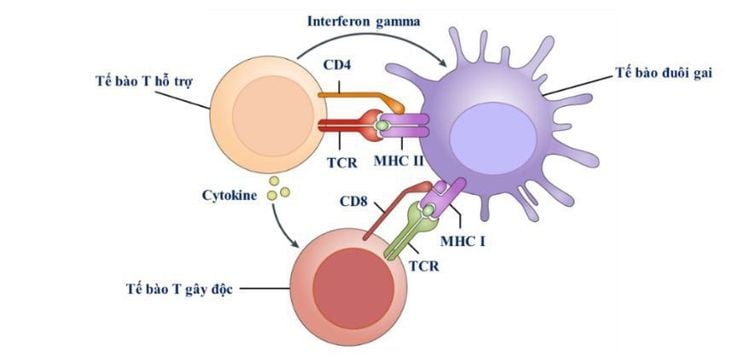
4.1 The pathogenesis of graft-host disease The pathogenesis of graft-host disease is not fully understood, but it can be triggered by destruction of host tissues through a number of factors. Different mechanisms involve donor cytotoxic T cells, natural killer cells, enteric bacterial antigen cross-reactivity, and release of cytotoxic agents following the interaction. interaction between host and donor cells.
Koyama et al suggested that graft-host disease is initiated by the interaction between the antigen-presenting cells of the recipient and the donor T cells. After transplantation, these antigen-presenting cells are modified by cell model signals derived from the gut microbiota. Gastrointestinal dendritic cells are activated in the colonic mucosa, leading to the development of graft-host disease.
4.2 Histological features of gastrointestinal graft-host disease Graft-host disease of the gastrointestinal tract is characterized by crypt cell apoptosis. This is a histological feature also described in other disorders, associated with immunoregulatory dysregulation and IBD, such as MMF colitis. However, the absolute number of apoptotic cells can be significantly higher in graft-host disease than in MMF colitis. Furthermore, among other histologically characteristic features of GVHD are neuroendocrine cell proliferation, which may be a compensatory response to cell loss, periportal inflammatory infiltrates, and cell loss. cell crypt cell. The histological features of chronic inflammation are similar to those described in inflammatory bowel disease and MMF colitis.
4.3 Treatment of graft-host disease Graft-host disease treatment includes methylprednisolone and immunosuppression with the aim of killing activated donor-derived lymphocytes. Simultaneously delete donor-derived lymphocytes with the host's innate immune system.
Currently, Vinmec International General Hospital has introduced Tacrolimus into the care and treatment system, to ensure that patients can use the appropriate tacrolimus dose regimen to optimize treatment effectiveness, minimize the risk of kidney transplant rejection as well as limit the unwanted effects of the drug. Therefore, the hospital will help patients after kidney transplant improve their quality of life and maintain the daily routine that the patient used to have.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References Gioco R, Corona D, Ekser B, Puzzo L, Inserra G, Pinto F, Schipa C, Privitera F, Veroux P, Veroux M. Gastrointestinal complications after kidney transplantation. World J Gastroenterol 2020; 26(38): 5797-5811 [PMID: 33132635 DOI: 10.3748/wjg.v26.i38.5797]