This is an automatically translated article.
The article was professionally consulted with Master, Doctor Pham Van Hung - Department of Medical Examination & Internal Medicine - Vinmec Da Nang International General Hospital.Ventricular arrhythmias are one of the most common types of cardiac arrhythmias. The variable heart rate originates supraventricularly with different foci of pacing, mainly originating in the atria. The disease has many causes and is mainly due to cardiovascular diseases.
1. Causes of ventricular arrhythmias
Ventricular arrhythmia is a state of variable rhythm with different pacing foci originating in the supraventricular, usually originating in the atria. There are many causes leading to ventricular arrhythmias such as from existing cardiovascular diseases, genetics, or unhealthy lifestyle.Common diseases that cause ventricular arrhythmias are:
Myocardial ischemia Heart failure Congenital heart disease Primary ventricular dysrhythmias Sudden neonatal death syndrome Cardiomyopathy: dilated, hypertrophic cardiomyopathy Coronary artery Right ventricular dysplasia Supraventricular arrhythmias are diverse, most patients are asymptomatic. Thus, the classification of supraventricular arrhythmias is based on the characteristics of the onset of the disease in the atria. The diagnostic method for supraventricular arrhythmias is mainly based on the electrocardiogram (ECG).
2. Classification of ventricular arrhythmias
2.1 Atrial extrasystoles ephedrine,... Extrasystoles can also be a manifestation of cardiopulmonary disease, particularly common in patients with chronic obstructive pulmonary disease. Patients usually present with palpitations.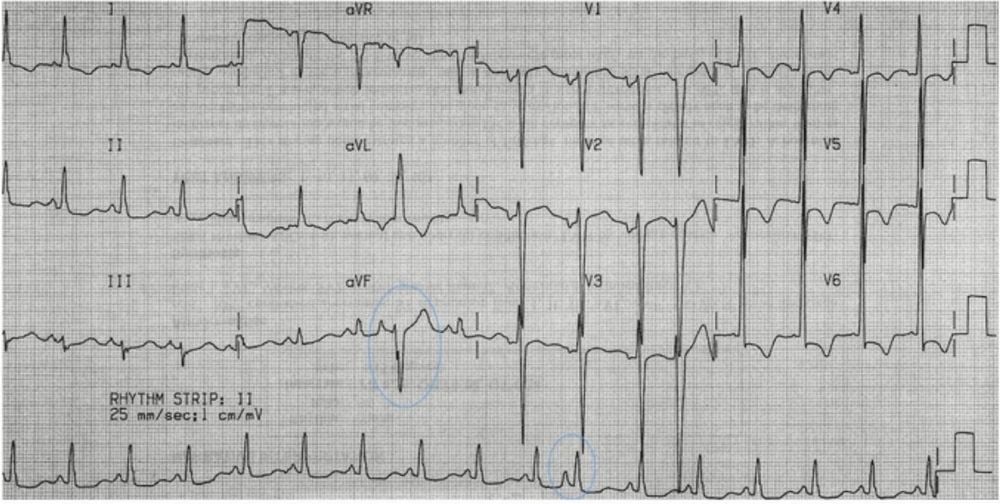
2.2 Atrial Tachycardia Atrial tachycardia is a rapid and persistent pattern of irregular heart rhythms that originate in a single focal spot in the atria. The heart rate is usually 150-200 beats/min. However, in the case of very tachycardia, the cause may be atrioventricular node dysfunction or digitalis toxicity leading to atrioventricular block. As a result, the supraventricular heart rate may be slower. Mechanisms include increased atrial automaticity and intra-atrial re-entry.
Atrial tachycardia is a rare condition that accounts for only about 5% of all types of ventricular arrhythmias. The disease is common in patients with structural heart disease. Other causes include atrial irritation, eg pericarditis caused by digoxin use, or alcohol and toxic gases.
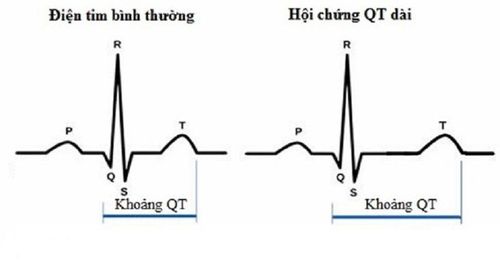
Symptoms often resemble those of other tachycardia arrhythmias. The method of diagnosis of atrial tachycardia is an electrocardiogram, which has a P wave with a different shape than that of a sinus P, which precedes the QRS complex. However, the P wave can also be masked by the T wave of the preceding complex. Parasympathetic stimulation can reduce heart rate, so that the presence of P waves that are not observed during tachycardia can be more clearly observed. Because the atrioventricular node is not a component of the arrhythmia circuit, parasympathetic stimulation testing usually does not terminate atrial tachycardia.
Treatment of atrial tachycardia includes treating the cause and reducing the ventricular rate response using beta-blockers or calcium channel blockers. Tachycardia can be stopped by cardioversion. Drugs that relieve and maintain sinus rhythm are class Ia, Ic, or III antiarrhythmic agents. If non-invasive treatments are not effective, over-frequency pacing and ablation may be necessary for relief.
2.3 Multifocal atrial tachycardia Multifocal atrial tachycardia is a complete arrhythmia. It is caused by various foreign pacing foci in the atria randomly pacing. Patients with multifocal atrial tachycardia will have a heart rate greater than 100 beats/min except for rate criteria. Other diagnostic criteria are similar to those of wandering atrial rhythm. Patients often present with very rapid ventricular arrhythmias.
Multifocal atrial tachycardia can be seen in lung disease such as chronic obstructive pulmonary disease, but can also be caused by heart disease such as coronary artery disease or electrolyte disturbances such as hypokalemia. The main method of treatment is to treat the underlying disease.

On the electrocardiogram is a regular rhythm, the QRS complex is normal without P waves or there may be a retrograde P wave just before or immediately after the QRS complex. Non-paroxysmal junctional tachycardia should be differentiated from paroxysmal supraventricular tachycardia. Treatment of the disease is the main cause.
2.5 Wandering atrial rhythm Vagrant atrial rhythm, also known as multifocal atrial arrhythmia, is a complete arrhythmia caused by multiple foci of foreign pacing in the atria spontaneously pacing. By definition, the heart rate is usually less than 100 beats per minute. This form of arrhythmia usually occurs in patients with pulmonary disease and hypoxia, theophylline toxicity, acidosis.
On the electrocardiogram, there are many different P wave patterns and more than 3 points. The differential diagnosis between wandering atrial fibrillation and atrial fibrillation should be based on the shape of the P on the electrocardiogram. The treatment for wandering atrial fibrillation is to treat the cause.
In summary, ventricular arrhythmia is one of the common and variable arrhythmias with different pacing foci originating in the supraventricular and usually in the atria. There are many causes of ventricular arrhythmias, mainly due to pre-existing cardiovascular diseases. Most patients have no symptoms, so diagnosis by electrocardiogram. Prolonged ventricular arrhythmias can be dangerous to the patient's health, so when there are abnormal symptoms, it is necessary to immediately seek medical attention for diagnosis and appropriate treatment.
Therefore, with early diagnosis of cardiovascular disease will help detect and promptly treat, avoid dangerous complications that may occur.

Especially, at Vinmec, there is also a Hybrid Operating Room with state-of-the-art equipment such as DSA angiography machine, integrated anesthesia machine that brings the highest efficiency in the treatment of cardiovascular diseases with modern minimally invasive techniques. most encroaching.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.