This is an automatically translated article.
Article by Doctor Pham Anh Tuan - Vinmec Institute of Stem Cell and Gene Technology
Despite improvements in treatment, non-small cell lung cancer patients still suffer severe damage leading to recurrence and death. The 5-year survival rate is only 10-15% and this is considered a hindrance in diagnosis.
Non-small cell lung cancer (NSCLC) is the most common form of lung cancer with about 85% of cases and is classified into 2 subtypes, squamous cell carcinoma (SCC) and epithelial cell carcinoma. tissue (adenocarcinoma-AC). SCC accounts for 20-30% of lung cancers and is more common in elderly men and is associated with smoking, while AC is more common in female patients and is not related to smoking.
Recently, studies have shown that TDEs (tumor-derived exosomes) contribute to cancer progression because they provide autocrine (involved in cell secreted components) and paracrine (cellular) signals. hormone-related) in the tumor ecosystem activates an epithelial-mesenchymal signaling program in melanoma cells.
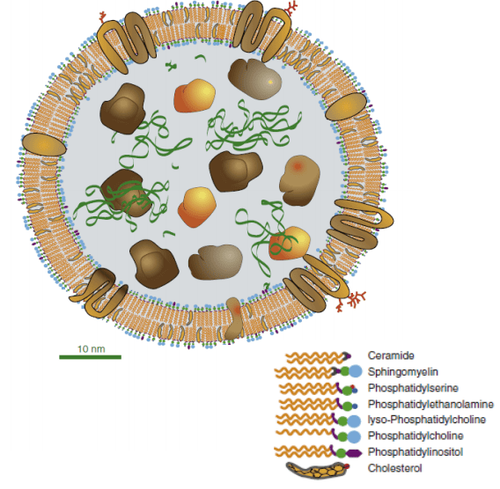
Cấu trúc của một exosome có kích thước trung bình (đường kính khoảng 60 nm)
TDEs are available in the blood and they contain valuable tumor marker proteins (such as EGFR, KRAS, RAB-family proteins). Thus, the proteins in the exosome can be quite a good reflection of the pathological stages involved. The separation of exosomes and their clinical use is considered a non-invasive diagnostic or monitoring procedure for cancer patients especially NSCLC because the possibility of finding primary cancerous tissue is very difficult in most patients. this patient. At the same time, the proteins in the exosome are protected from degradation by proteinases and thus can be identified in circulating blood (plasma, serum).
This study using proteomics has predicted that exosome proteomes are valuable diagnostic markers for non-small cell lung cancer. Although proteomic changes of exosomes have been described in many malignancies, little is known about NSCLC metastases. This study was conducted on serum samples of NSCLC patients and healthy controls. Tandem mass tags (TMTs) combined with multidimensional liquid chromatography and mass spectrometry analysis were used by the team to profile the serum samples.

Ung thư phổi không tế bào nhỏ
Quantification of the proteome, evaluation of specific signaling pathways and functional subtypes for metastatic and non-metastatic lung cancer patients as well as controls were conducted. Out of a total of 628 proteins, 552 proteins were quantified. Bioinformatics analysis identifies valuable proteins involved in biological functions and signaling pathways involved in metastasis. Furthermore, the LBPs (lipopolysaccharide-binding proteins) in exosomes were found to be quite different between metastatic and non-metastatic patients (Area under curve-AUC 0.803 with 83.1% sensitivity, specificity). 67%, P<0.0001). Meanwhile, circulating LBPs were also significantly different between these two groups of NSCLC patients (AUC 0.683 with sensitivity 79.5%, specificity 47.2%, P=0.005).
This new finding provides a reliable proteome map for metastatic non-small cell lung cancer research to confirm that metastatic and non-metastatic NSCLC patients are differentiated through the sample. serum, non-invasive.
References:
Kushnir M.M., Rockwood A.L., Bergquist J., Liquid chromatography-tandem mass spectrometry applications in endocrinology, 2010, Mass Spectrom Rev, 29: 480–502
Oyben T., Expanded newborn screening and confirmatory follow- up testing for inborn errors of metabolism detected by tandem mass spectrome- try, 2013, Clin Chem Lab Med, 51: 157–76.
Rousseau F, Giguère Y, Berthier MT et al., Tandem Mass Spectrometry Applications and Principle, 2012, InTech, 30, 722–50
Herman J, Shushan B: Clinical applications, Tandem mass spectrometry applications and principle, 2012, InTech, 29, 673–721
Ning W. et al., Circulating exosomes contain protein biomarkers of metastatic non-small-cell lung cancer, 2018, Cancer Science, 109: 1701-1709 .