This is an automatically translated article.
The article was written by Specialist Doctor I Nguyen Thi Minh Thuyen - Pathologist, Pathology Department - Vinmec Danang International General Hospital.Cervical cancer is a malignant disease for which there is no specific treatment. Learning about the risk factors and causes of cervical cancer will help each person take more effective preventive measures.
1. Risk factors for cervical cancer
A risk factor is anything that affects the likelihood of getting a disease. Different cancers have different risk factors. For example, excessive sun exposure is a risk factor for skin cancer. Smoking is a risk factor for many cancers. But having one risk factor, or even several, doesn't mean you'll get the disease.Several risk factors can increase your chances of getting cervical cancer. Women without any of these risk factors rarely get cervical cancer. Although these risk factors may increase the incidence of cervical cancer, many women with these risk factors do not develop the disease.
When you think about risk factors, it helps you focus on the things you can change or avoid (like smoking or human papillomavirus infection), rather than the things you can't change (like age and family history). However, it is important to know about risk factors that cannot be changed, because women with these factors need regular screening tests to detect cervical cancer early.
1.1. Modifiable risk factors
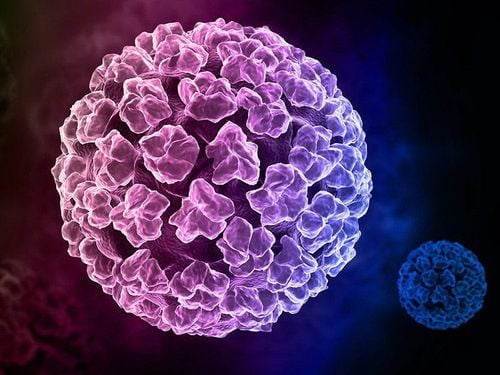
1.1.1 Human papillomavirus (HPV) infection Human papillomavirus (HPV) infection is the most important risk factor for cervical cancer. HPV is a group of more than 150 related viruses. Some of them cause papillomas, most commonly known as warts.HPV can infect cells on the surface of the skin, and those lining the genitals, anus, mouth, and throat, but not in the blood or internal organs such as the heart or lungs. HPV can be spread from person to person during skin-to-skin contact. One way HPV is spread is through sexual contact, including vaginal, anal, and even oral sex. Different types of HPV cause warts on different parts of the body. Common warts on hands and feet; Others tend to have warts on their lips or tongue. Certain types of HPV can cause warts on or around the female and male genitalia and in the anal area. These are called low-risk types of HPV because they are rarely associated with cancer.
Other types of HPV are called high-risk HPV because they are closely associated with cancer, including cervical, vulvar and vaginal cancers in women, penile cancer in men, and cancer of the penis in men. anus, mouth, and throat in both men and women.
HPV infection is common and in most people the body clears it up on its own. Sometimes, however, a viral infection doesn't go away and becomes chronic. Chronic infection, especially when it's caused by certain types of high-risk HPV, can be the cause of some cancers, like cervical cancer.
Although there is currently no cure for HPV infection, there are ways to treat warts and the abnormal cell growth that HPV causes. In addition, the HPV vaccine can help prevent infection with some types of HPV and some cancers associated with those types.
1.1.2 Sexual history Several factors related to sexual history can increase the risk of cervical cancer. This risk is most likely influenced by increased exposure to HPV.
Having sex at a young age (especially under 18) Having multiple sex partners Having one high-risk partner (one who has HPV or has multiple sex partners)

Bệnh tình nhiễm HPV dẫn đến nguy cơ gây bệnh ung thư cổ tử cung
Women who smoke are twice as likely to develop cervical cancer as non-smokers. Tobacco products have been found in the cervical mucus of women who smoke. Researchers believe these substances damage the DNA of cervical cells and may contribute to cervical cancer. Smoking also makes the immune system less effective at fighting HPV infections.
1.1.4 Weakened Immune System Human immunodeficiency virus (HIV), the virus that causes AIDS, weakens the immune system and puts the body at higher risk of HPV infection.
The immune system plays an important role in destroying cancer cells and slowing their growth and spread. In HIV-infected women, precancerous lesions of the cervix may develop into invasive cancer more quickly than usual.
Another group of women at increased risk for cervical cancer are those taking drugs that suppress the immune response, such as those being treated for autoimmune disease (a disease in which the immune system views the body's tissues as possible). themselves as foreign objects and attack them, viewing them as pathogens ) or people who have received organ transplants.
1.1.5 Chlamydia Infection Chlamydia is a relatively common bacteria that can be transmitted through the genital system, through sexual contact. Women infected with Chlamydia often have no symptoms and they may not know they are infected unless they are screened during a pelvic exam. Chlamydia infection can cause pelvic inflammatory disease, leading to infertility.
Some studies have shown a higher risk of cervical cancer in women whose cervical mucus and blood tests have evidence of Chlamydia infection (past or present). Some research indicates that Chlamydia bacteria can help HPV grow and live in the cervix and may increase the risk of cervical cancer.
1.1.6 Long-term use of oral contraceptives There is evidence that long-term use of oral contraceptives (OCs) increases the risk of cervical cancer. Research shows that the risk of cervical cancer is increased in women who use OCs long-term. Women should discuss with their doctors whether the benefits of using OCs outweigh the potential risks.
1.1.7 Multiple pregnancies Women who have had 3 or more pregnancies have a higher risk of cervical cancer. It is thought that this is probably due to the increased exposure to HPV with sexual activity. In addition, studies have shown hormonal changes during pregnancy can make women more susceptible to HPV infection or the formation of cancer. Others think that pregnant women may have weaker immune systems, facilitating HPV exposure and cancer development.
1.1.8 Young Pregnancy Age Women under 20 years of age with their first full-term pregnancy are more likely to develop cervical cancer than pregnant women who are 25 years of age or older.
1.1.9 Economic Status Many low-income women do not have easy access to adequate health care services, including cervical cancer screening with Pap tests and HPV testing. This means they may not be screened or treated for cervical cancer.
1.1.20 Diets low in fruits and vegetables Women whose diets do not include enough fruits and vegetables may have an increased risk of cervical cancer.

Ăn ít trái cây khiến phụ nữ có thể bị ung thư cổ tử cung.
1.2. Risk factors that cannot be changed
Diethylstilbestrol (DES) - DES is a hormonal medication that was given to some women between 1938 and 1971 to prevent miscarriage. Women whose mothers used DES (during pregnancy) have an increased risk of developing clear-cell adenocarcinoma of the vagina or cervix. These cancers are extremely rare in women who are not exposed to DES. There is about 1 case of clear cell carcinoma of the vagina or cervix in every 1,000 women whose mothers used DES during pregnancy. This means that about 99.9% of "DES daughters" do not have these cancers.
- DES-associated clear cell carcinoma is more common in the vagina than the cervix. The risk appears to be greatest in women whose mothers took the drug during the first 16 weeks of pregnancy. The average age of women diagnosed with DES-associated clear cell carcinoma is 19 years. Since the use of DES during pregnancy was banned by the FDA in 1971, even the youngest daughters are almost 50 years old - past the age at greatest risk. However, there is no age limit when these women feel safe about DES-related cancers. Doctors don't know exactly how long these women will remain at risk.
- “DES daughter” may also increase the risk of HPV-associated squamous cell carcinoma and pre-cancer of the cervix.
Have a family history of cervical cancer Cervical cancer can run in some families. If your mother or sister had cervical cancer, your chances of getting it are higher if no one in your family has had it. Some researchers suspect that some rare cases of this familial tendency are caused by an inherited condition that makes some women less resistant to HPV infection than others. In other cases, women in the same family as the diagnosed patient may be more likely to have one or more other non-genetic risk factors.
1.3. Factors that may reduce the risk
Use of an IUD Some studies show that women who have ever used an IUD have a lower risk of cervical cancer. This was seen even in women who had been using the IUD for less than a year, and the protective effect remained after not using the IUD.
IUDs have some risks, and women interested in using an IUD should first discuss the risks and benefits with their doctor. Because, a woman with multiple sex partners should use condoms to reduce her risk of STIs no matter what other form of contraception she uses.
2. Prevention of cervical cancer
There is no way to completely prevent cancer. But there are things you can do to reduce your risk. The 2 most important things you can do to prevent cervical cancer are to get the HPV vaccine if you qualify and get tested as recommended by experts.
The most common form of cervical cancer stems from precancerous changes and there are ways to stop them from growing. The first is to find and treat precancerous lesions before they develop into invasive cancers, and the second is to prevent precancerous lesions.
2.1. Cervical pre-cancer detection
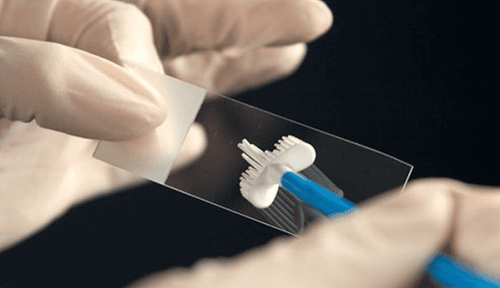
One obvious way to prevent cervical cancer is to have a screening test. Screening is tests to find conditions that can lead to cancer and find precancerous lesions before they can become invasive cancer. The Pap test (or Pap smear) and the human papillomavirus (HPV) test are specific tests used during cervical cancer screening. If precancerous is found, it can be treated, keeping it from becoming cervical cancer.
A Pap test or smear is a method used to collect cells from the cervix, which are thoroughly analyzed with a microscope in a laboratory to look for cancer and pre-cancers. It is important to know that most invasive cervical cancers are found in women who do not have regular Pap tests. A Pap test can be done during a pelvic exam, but not all gynecological tests include a Pap test. The HPV test may be done at the same time as the Pap smear. The HPV test checks for HPV infection, which is one of the possible causes of pre-cancer.

Xét nghiệm PAP giúp hát hiện tiền ung thư cổ tử cung
2.2. Things to do to prevent pre-cancer and cancer
Based on age, overall health, and individual risk for cervical cancer, there are several things that can be done to prevent pre-cancers and conditions that lead to pre-cancers.
Get the HPV vaccine The vaccine can protect young people against some HPV infections. These vaccines protect against infection with the most common types of HPV associated with cancer, as well as some types that can cause genital and anal warts.
These vaccines only work to prevent HPV infection – they do not treat an already existing infection. That's why, to be most effective, the vaccine is recommended before exposure to HPV (like sex). These vaccines help prevent pre-cancers and cervical cancer. Some HPV vaccines are also approved to help prevent other types of cancer and genital and anal warts.
These vaccines require several shots, and side effects are usually mild. The most common is redness, swelling, and brief soreness at the injection site. Rarely, in young people, fainting may occur shortly after the injection.
The Centers for Disease Control and Prevention recommends:
HPV vaccination starting at age 11 or 12 (or can be given as early as age 9). If unvaccinated, everyone can be vaccinated by age 26. It's important to know that getting vaccinated as you age is less effective at reducing cancer risk. Vaccination is not recommended for people over the age of 26. However, some unvaccinated adults aged 27 to 45 years may decide to get the HPV vaccine after talking with their healthcare provider about the risks of new HPV infection and the benefits. possible benefits of vaccination. HPV vaccination in this age group has less benefit. It's important to know that no vaccine completely protects against all strains of cancer-causing HPV, so routine cervical cancer screening is still needed.
Limit exposure to HPV HPV is transmitted from person to person during skin-to-skin contact with infected areas of the body, including vaginal, anal, and oral sex . There's even a chance that a genital infection is spread through hand-to-genital contact.
Also, HPV infection seems to be able to spread from one part of the body to another. This means that HPV infection can start in the cervix and then spread to the vagina and vulva.
It can be very difficult not to be exposed to HPV. HPV infection can be prevented by not allowing others to have contact with the anal or genital area, but even then you become infected for unknown reasons.
Limiting the number of sexual partners and avoiding sex with people who have had many other sexual partners can reduce the risk of being exposed to HPV. Remember that HPV is very common, and someone can have HPV for many years and still have no symptoms. So it is possible that these people carry HPV and transmit it without knowing it.
Use condoms Condoms help protect against HPV, but they don't completely prevent infection, because they don't cover all HPV-infected areas, such as the skin of the genitals. genital or anal area. However, condoms help protect against HPV, and they also protect against HIV and some other sexually transmitted infections.

Hãy sử dụng bao cao để chống lại HPV
No smoking No smoking is necessary to reduce the risk of pre-cancer and cervical cancer.
To meet the needs of women for gynecological cancer screening, Vinmec International Hospital currently provides a screening package and early detection of gynecological cancer, helping to detect 4 diseases early: Cancer cervical cancer, breast cancer, uterine cancer and ovarian cancer even if the patient has no symptoms.
The subjects who should use the Gynecological cancer screening and early detection package include:
Female customers, over 40 years old Customers wishing to be able to screen for pathology of breast-gynecological cancer (neck) uterus, uterus, ovaries) Customers at high risk of cancer – especially customers with a family history of breast cancer, gynecology Women of reproductive age, perimenopause Menopause and menopause Women are having symptoms of breast cancer, gynecology such as: pain in the breast, lump in the breast, bleeding outside the menstrual cycle, abdominal pain, etc... To register for an examination and treatment at Vinmec International General Hospital You can contact Vinmec Health System nationwide or register online HERE.
Articles refer to the source: American Cancer Society
MORE:
Signs of cervical cancer women do not ignore Cervical cancer treatment in stages Causes of cervical cancer What is bow?