This is an automatically translated article.
Oral mucosa is the mucosal layer that covers the oral cavity and tongue. For some reason, this mucosal layer is damaged, which can lead to ulcers, pus or not, causing pain and difficulty for the patient to eat, drink and talk. What causes oral mucositis?
1. What is the cause of oral mucositis?
Mucositis can appear anywhere in the digestive tract, including the oral cavity, causing the patient to feel pain and difficulty in eating and communicating daily.
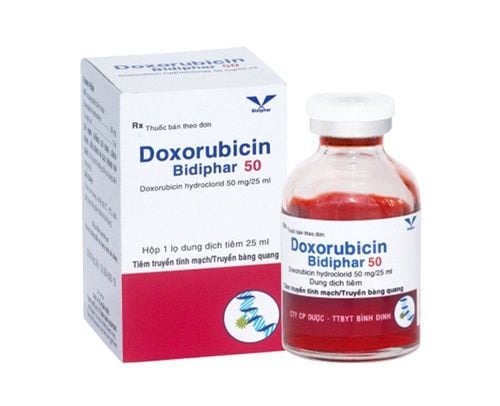
Oral mucositis often occurs in patients undergoing cancer treatment with methods such as chemotherapy, radiation therapy in the head - chest or neck area, patients with bone marrow transplants, stem cell transplants. .. About 40% of cancer patients undergoing chemotherapy will have inflammation of the lining of the tongue or mouth. This risk is higher in patients treated for cancer in areas such as the head, neck or chest. There are also other factors that increase the inflammation of the oral mucosa in cancer treatment patients such as:
Female gender; History of dry mouth before and during cancer treatment; Being dehydrated; Have a chronic disease such as kidney disease or diabetes; Sudden unexplained drop in body mass index; Poor oral health; Smoking or using alcohol. The anatomical structure of the digestive system includes the mouth, pharynx, esophagus, stomach, and intestines. In which, the mucosa is the membrane that covers the surface, made up of cells capable of rapidly dividing and plays a role of protecting and moisturizing the above organs. Patients with oral mucositis often start with cancer treatment that damages the cells and prevents them from dividing as they should. This leads to the cells having difficulty in repairing and protecting themselves inside the mouth and throat, and stimulates the body to create an inflammatory response to try to protect itself. There are many cancer chemotherapy drugs available today that have a risk of causing oral mucosal ulcers, especially when used in higher doses or more often. For example, weekly treatment with 5-fluorouracil (5-FU) was identified as one of the causes of mouth ulcers.
Radiation therapy for head and neck cancers can also cause inflammation of the lining of the tongue, mouth, throat, and esophagus. Usually, mucosal lesions usually appear in the 3rd or 4th week of radiation therapy and worsen during radiation therapy. Therefore, prophylactic treatment should be initiated from the beginning of radiation therapy with the aim of delaying and reducing the extent of mucosal damage. However, the damage caused by oral mucositis can slowly recover after the end of radiation therapy, so the patient should maintain the habit of gargling until the ulcers are completely healed. In addition, statistics show that patients who are being treated for hematological malignancies have a higher risk of mouth ulcers.
Có nhiều nguyên nhân khác nhau có thể gây viêm niêm mạc miệng
In addition to cancer-related oral mucositis, the habit of drinking alcohol or smoking is considered one of the risk factors for the disease because this bad habit makes the mucosa easily dry, leading to an increased chance hurt. At the same time, poor oral hygiene habits or wearing ill-fitting dentures can also increase your risk of mouth problems, including canker sores.
2. What are the symptoms of oral mucositis?
Inflammation of the lining of the tongue and mouth presents many different symptoms, such as:
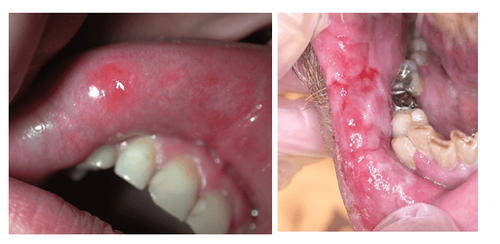
Dry mouth ; Thicker saliva; Increased sebum secretion; The part of the gums that becomes shiny, swollen, or red; The tongue may appear white, soft, or pus-filled; The appearance of sores accompanied by bleeding in the mouth; Feeling of mild heat when eating; Pain when talking or swallowing. Patients with oral mucositis often present with relatively clear symptoms in the early stages of cancer treatment, so doctors can diagnose this condition during the first 1-2 weeks of radiation therapy or within 3 days of treatment. perform chemotherapy. To make an accurate diagnosis, the doctor will examine and evaluate the symptoms in the oral mucosa, combined with a history of previous diseases.
3. Interventions for oral mucositis
3.1 Monitor the oral cavity regularly Patients with oral mucositis should regularly check the oral cavity every day by a very simple measure of standing in front of a mirror and using a lamp to shine in the mouth to observe the inside. If you notice unusual signs such as ulcers, pus, areas of congestion or pseudomembranous... then quickly notify the doctor for timely handling measures.
3.2. Maintain a sufficiently moist and clean oral cavity Clean teeth with a brush every day: Note to limit further damage in inflamed mucosa sites, patients should use a soft-bristled brush and ensure quality. In case of too severe oral mucositis, it is possible to just use soft gauze to clean the teeth; Limited or no flossing because of the potential for pain or bleeding; Gargle with 0.9% physiological saline or 1.5% hydrogen peroxide solution (1 part hydrogen peroxide diluted with 3 parts water) for 1-2 minutes, every 2 hours. If the pain caused by mucositis is more severe, it is necessary to gargle once every hour; Use a quality moisturizer; Add enough water every day (about 1.5 - 2 liters), when drinking, you should take small sips several times a day (15 - 20 minutes at a time).

Chỉ nha khoa cần được hạn chế sử dụng khi bạn bị viêm niêm mạc miệng
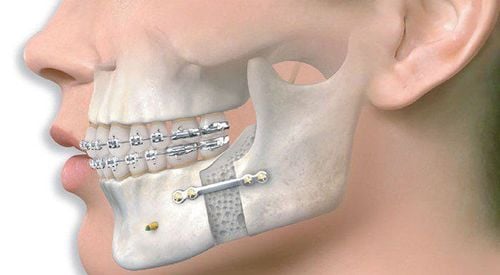
3.3 Notes on diet Absolutely limit spicy, hot, sour, too hard or acidic foods; Do not use alcoholic beverages such as wine, beer; The diet is fortified with protein-rich foods such as meat, eggs, milk...; Fortified with essential vitamins and minerals daily. 3.4. Patients with oral mucositis that are more painful and do not improve will be prescribed pain relievers by the doctor about 1.5-2 hours before meals or use a cotton swab to dip the anesthetic solution on the areas of the mouth. sores; If the ulcer is accompanied by bleeding, the doctor will instruct the patient to use a cotton swab soaked in cold water to apply pressure to the bleeding point. Besides, people with oral mucositis can gargle with cold water to limit bleeding; In case of prolonged mucosal ulceration, it is necessary to use appropriate analgesics, limit exposure or bone necrosis with hyperbaric oxygen;
4. Complications of oral mucositis
Inflammation of the oral mucosa can lead to a number of complications as follows:
Decrease or loss of appetite, resulting in a lack of essential nutrients; Increased risk of bacterial, viral or fungal infections, especially blood infections; Causes cancer treatment to be delayed or delayed, which in turn leads to other serious side effects;
5. How to prevent oral mucositis?
Proper hygiene and brushing daily, combined with rinsing with the right solution for a more comprehensive hygiene; Should use toothpaste containing fluoride; No smoking; Drink enough water daily; Strengthens lips and mouth to keep warm; Build and maintain a healthy, scientific diet, avoiding spicy, hot, too salty, too hard or crunchy foods. Also, limit or avoid hot, carbonated or alcoholic beverages; Gradually reduce the amount of sugar consumed each day. If the above methods do not improve your condition, visit a medical facility, your doctor will examine you and determine the most useful treatment for you. Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading doctors, modern equipment and technology, but also stands out for its examination and consulting services. and comprehensive, professional medical treatment; civilized, polite, safe and sterile medical examination and treatment space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.