This is an automatically translated article.
Posted by Specialist Doctor II Pham Thi Van Hanh - Pediatric Center - Vinmec Times City International HospitalChildren exposed to HIV from their mothers will have special care and treatment procedures. It is important to identify the child's condition, explain it to the family, and provide instructions on how to care for the child to help him or her grow up healthy.
1. Outline
HIV/AIDS is a chronic infection caused by human immunodeficiency virus (HIV) infection. The disease has a long asymptomatic latent phase. Severe manifestations in the late stage are acquired immunodeficiency syndrome - AIDS (Acquired Immune Deficiency Syndrome)Origin: HIV-1 and HIV-2 viruses, belonging to the RETRO VIRIDAE family. Transmission route: Via 3 routes: blood. , sexual transmission and mother-to-child transmission Epidemiology: Vietnam detected the first HIV infection in 1990. Up to September 2017, there were 208, 371 people infected with HIV, including 90,493 AIDS patients. The incidence is increased in women of childbearing age. Early intervention from the time of pregnancy will help reduce the HIV infection rate for babies born to HIV-infected mothers from 30 -40% to only 1-2%.
2. Purpose of management, care and monitoring of children exposed to HIV
Children born to HIV-infected mothers are identified early. Help children access antiretroviral treatment early, reduce severity and mortality of HIV-infected children. Early diagnosis of HIV infection and early ART reduce mortality by 76% and HIV progression by 75%. HIV treatment is more difficult if the child is already in a severe condition. Improve physical and mental development for HIV-infected children. Children exposed to HIV from their mothers need to be cared for, supported, monitored, tested for early diagnosis, so that they can receive vital interventions such as cotrimoxazole prophylaxis and ART as soon as their status is confirmed. infection
Trẻ có phơi nhiễm với HIV từ mẹ cần được chăm sóc, hỗ trợ, theo dõi, xét nghiệm chẩn đoán sớm để sớm được điều trị
3. Subjects and process of care and treatment for HIV-exposed children at health facilities
3.1 Subjects of management and care Children under 18 months of age born to HIV-infected mothers (exposure) will be referred from an obstetric facility/HIV transmission prevention program to a pediatric HIV care and treatment facility Children under 18 months of age with suspected HIV infection or clinically diagnosed severe HIV/AIDS disease and tested positive for anti-HIV antibodies. (These children are born to mothers who may not have known HIV status or have known HIV status before but have not been adequately counseled on care and treatment for the child. 3.2 Implementation of follow-up procedures. child admission All HIV-exposed children under 18 months of age are admitted to the treatment facility Children and caregivers are instructed to register for long-term care and make a profile..4. Contents of management, care and treatment for children exposed to HIV
Counseling, initial assessment and record-keeping of care managementCounseling and support:
Identifying caregivers, assessing understanding to implement the contents to be consulted Counseling for mental support management, care, and monitoring of exposed children Introduction of services for HIV-exposed children in the facility (early diagnosis, opportunistic infection prevention, nutrition and ART) .. Initial assessment:
Ask the family's HIV history, mother's history of ARV drug use, nurture, prevention, vaccination, disease since birth, developmental milestones according to age, source of tuberculosis in family.
Examination to assess the child's health status: vital signs, height, weight and head circumference of the child. TB screening, physical and mental development assessment. Physical examination and laboratory tests necessary to diagnose OIs and other diseases,
Clinically diagnose severe HIV/AIDS when antibody tests are positive and one of the following clinical stage 4 diseases is present. PCP pneumonia, Toxoplasma encephalitis, Cryptococcal meningitis, unexplained severe emaciation, extrapulmonary tuberculosis, esophageal candidiasis or at least 2 of 3 manifestations:
Oral thrush (in children) over 1 month old) Severe bacterial pneumonia Severe sepsis These children need to have their medical records completed, ART, and PCR tested to diagnose HIV infection as soon as possible

Khám đánh giá tình trạng sức khỏe của trẻ thông qua các thông tin: Dấu hiệu sinh tồn, chiều cao, cân nặng và vòng đầu của trẻ
5. Early diagnosis of HIV infection
Subjects: Children under 18 months of age, because maternal antibodies cross the placenta, antibody tests are false positive. These children need to be tested according to their own proceduresChildren born to HIV-infected mothers < 18 months of age Children with suspected HIV infection or clinically diagnosed severe HIV/AIDS disease and tested for anti-HIV antibodies (+) . Time of testing: When the baby is 4-6 weeks old or right at the first visit at a care and treatment facility. 5.1 Purpose Early identification of HIV infection status in children under 18 months of age. Timely ART for all HIV-infected children. Early diagnosis of HIV infection and early antiretroviral therapy to reduce HIV mortality and progression. Reduce stress for families and caregivers.
5.2 Testing methods Because anti-HIV antibodies are transmitted from mother to child during pregnancy and persist for up to 18 months, to confirm HIV status early for HIV-exposed children under 18 months of age, testing must be performed. antigen detection test.
5.3 Procedure for HIV-exposed children < 9 months old: Do PCR test right away
Children with suspected HIV infection, clinically severe disease, children from 9 to under 18 months old: Do an anti-HIV antibody test first, if the result is positive do PCR
Pre-test counseling, order testing Risk of mother-to-child transmission of HIV and progression of HIV/AIDS. The benefits and necessity of early diagnosis of HIV infection and how to collect the sample, how to conduct the test and the time to return the results. Advice on infant feeding and the importance of 3-drug ART if nursing mothers
Assertion about confidentiality of test results
Tests Collect blood samples for testing with a dry blood drop kit (DBS), this is a simple blood sampling method, depending on the weight of the child, choose the appropriate injection site: heel, big toe or finger, blood is soaked into the DBS sheet,
Store, pack DBS sheets and transport patient samples by post to the Central Institute of Hygiene and Epidemiology and Pasteur Institute in Ho Chi Minh City
Post-test consultation and result handling Case of PCR test results positive
1st PCR test result is positive;
Current PCR test results, the need to repeat the test to confirm the child's HIV status, time to take the 2nd DBS sample. Psychological support; counseling on long-term care and treatment and ART for children. Counseling for the child's parents to take an HIV test if the parent's HIV status is unknown; and further support if needed. Immediate ARV treatment for the child, and at the same time take a dry blood sample and repeat PCR The second PCR test result is positive: Advise caregivers and continue ARV treatment. In case the PCR test result is negative: Explain what the test result means
Children who are not breastfed or who have stopped breastfeeding completely 6 weeks before the PCR test: The child is likely not HIV-infected, continue monitoring and testing for anti-HIV antibodies when the child is 18 months old. Children who are breastfeeding or who have stopped breastfeeding for less than 6 weeks: Children are still at risk of HIV infection through breast milk, how to monitor and test children. Counseling on infant feeding, the risk of HIV transmission through breast milk and the benefits of early ART for mothers, especially in cases where mothers continue to breastfeed.

Trẻ nhỏ dưới 18 tháng tuổi, do còn kháng thể ở mẹ sang qua nhau thai nên xét nghiệm kháng thể có dương tính giả
Content: Assessment of caregivers' feeding conditions
Counseling on nutritional and immunological benefits as well as the risk of HIV transmission when HIV-positive mothers choose to breastfeed, the risks and benefits benefits of using formula.
Provide information on feeding regimens for mothers to choose from:
Option 1: Breastfeeding Counseling on exclusive breastfeeding for the first 6 months and continued breastfeeding for up to 12 months with complementary foods Safe and appropriate supplementation, Counseling on the need for exclusive breastfeeding and educating mothers on proper breastfeeding and breast hygiene Advice on the benefits of ART for the mother and infection prevention HIV to the baby, even if the mother is breastfeeding If the mother develops AIDS symptoms while breastfeeding, counsel the mother to wean Option 2: Formula feed (AFASS) use formula milk as a substitute for children who do not have HIV or whose HIV status is unknown in the first 6 months when the following conditions are met:
The mother wishes to feed her baby with replacement milk Feeding her baby with milk substitute is feasible (milk can be purchased, clean water is available, ...) Mother has enough money to buy formula for her baby It is possible to buy milk in the long term It is safe to give her baby a substitute: It is possible: preparation ability milk and feed your baby safely

Mẹ có thể nuôi trẻ phơi nhiễm với HIV bằng sữa mẹ hoặc sữa công thức
6. Cotrimoxazole prophylaxis (CTX)
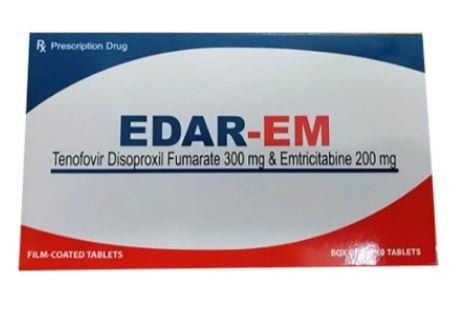
Advise on the importance of CTX prophylaxis for HIV-exposed children (P.Jiroveci pneumonia (PCP) is the leading UTI causing death in HIV-infected children under 1 year of age) Time of CTX treatment: from 4 -6 weeks of age or immediately thereafter, while awaiting PCR results. Stop taking after testing confirms HIV absence. Contraindications: Allergic to Sulfamid group Dosage: 5mg/kg/day according to Trimethoprim (TMP) CTX form used: 1ml syrup with 8mg TMP and 40mg SMX, CTX 240 pack with 40mg7. Vaccinations
Children exposed to HIV should be vaccinated on the same schedule as uninfected children. Delay vaccination with live vaccines in cases of clinically severe illness Delay BCG injection if the child is <2500 g; mother and child are not receiving antiretroviral therapy to prevent mother-to-child HIV transmission; Children with signs or symptoms of HIV infection
Trẻ phơi nhiễm HIV cần được tiêm chủng theo lịch như các trẻ không nhiễm
8. ARV treatment for children under 18 months of age
Prophylactic ART for nursing infants:ARV treatment for HIV-exposed children:
Immediate ARV treatment for children when the first PCR results are available (see early diagnosis of HIV infection) Immediate ARV treatment for children is available. clinical diagnosis of severe HIV disease with positive anti-HIV antibodies and PCR test to diagnose HIV infection
9. Monitoring the child at the care facility
Periodic examination, schedule follow-up examination for exposed children; Advise caregivers on the implications of management and monitoring for the child, to avoid losing track, until infection is confirmed for the child Assessing mental and physical development according to developmental milestones, Counseling for compliance treatment and monitoring treatment Child nutrition counseling, ARV treatment counseling for mothers, HIV diagnostic tests for children with negative PCR test results but still breastfeeding Monitor side effects if taking Medicines Teaching caregivers how to care for and monitor children at home10. Care, support and advice for carers
Identify the role of caregivers, ensure timely communication and follow-up, coordinate with health workers in the process of child care, especially in early diagnosis of HIV infection and timely ARV treatment.Carers receive advice and guidance on care and support for exposed children. Need to assess, identify caregivers' difficulties and advise solutions
Coordinate and refer to special support services
Monitor and care for children exposed to HIV from their mothers, help eliminate infection New HIV in children, improving the quality of life for HIV-infected children. Confirm HIV status in exposed children by PCR testing for children under 18 months as soon as possible, avoiding losing track. At the same time, ensure that HIV-infected children receive ART early, including those with clinical signs of severe HIV/AIDS in infants when HIV status cannot be confirmed. Guidelines for correct and safe child rearing.
Pediatrics department at Vinmec International General Hospital is the address for receiving and examining diseases that infants and young children are susceptible to: viral fever, bacterial fever, otitis media, pneumonia in children, ... With modern equipment, sterile space, minimizing the impact as well as the risk of disease spread. Along with that is the dedication from the doctors with professional experience with pediatric patients, making the examination no longer a concern of the parents.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.