This is an automatically translated article.
Article by Master, Doctor Mai Vien Phuong - Gastrointestinal endoscopist - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
If you have surgery to remove your pancreas, you can still live without it. However, you'll have to make lifestyle adjustments, take medications your doctor prescribes and monitor your blood sugar, and stay physically active on a daily basis.
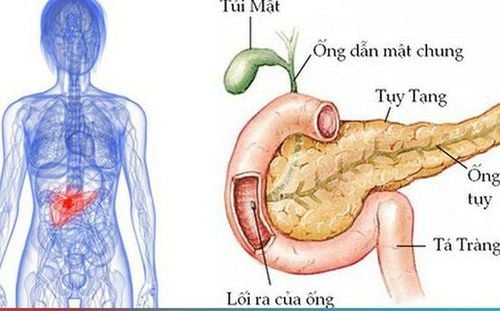
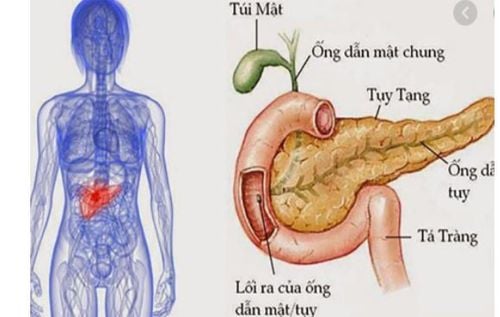
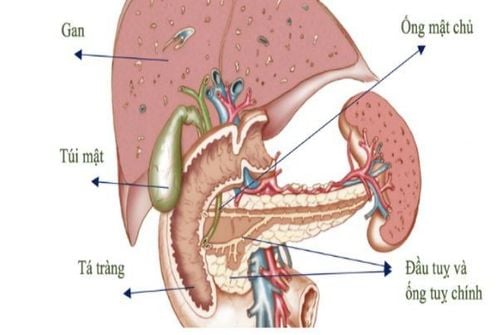
1. What is the pancreas?
The pancreas is located high in the abdomen, near the main veins and arteries. The pancreas has three parts, namely the head, body and tail of the pancreas.
This organ is responsible for making hormones such as insulin and digestive enzymes. Digestive enzymes and hormones produced in the pancreas travel from the pancreas to the duodenum through the pancreatic duct. If the pancreas produces hormones, it is called the endocrine pancreas, and the part that produces digestive enzymes is called the exocrine pancreas.
2. What is the function of the pancreas? 2.1. Exocrine function Every day, exocrine pancreas excretes about 1000ml of pancreatic juice. During meals, when looking, smelling, thinking about food or chewing and swallowing, about 20% of pancreatic juice can be secreted during the whole meal. After the food enters the stomach, it secretes 5-10% pancreatic juice, and when the food reaches the intestines it is 70% pancreatic juice.
Pancreatic juice contains many bicarbonate salts and enzymes that help digest most food, including:
Protein digesting enzymes (trypsin, chymotrypsin, elastase, carboxypeptidase). Glucose-digesting enzyme (amylase). Lipid digesting enzyme (lipase, phospholipase A2, cholesterol esterase) Nucleic acid digesting enzyme (ribonuclease, desoxyribonuclease). 2.2. Endocrine function The endocrine pancreas secretes many hormones into the bloodstream, the most important of which are glucagon and insulin.
Insulin has the effect of lowering blood sugar. Therefore, if there is a lack of insulin, it will cause an increase in blood sugar, which can lead to diabetes. In contrast, Glucagon has the effect of increasing blood sugar, enhancing the breakdown of gycogen in the liver into glucose in the blood.
Currently, surgical removal of the entire pancreas is rarely performed. However, if you have pancreatic cancer, severe pancreatitis, or damage to your pancreas from an injury, you may need to have your pancreas removed.
Thanks to new drugs, life expectancy after pancreatectomy is increasing. Therefore, your outlook will depend on the condition you have. One study found that the 7-year survival rate after surgery for people without cancers like pancreatitis was 76%. But for people with pancreatic cancer, the seven-year survival rate is 31 percent.
4. What do the cells of the pancreas do? The pancreas is a gland located in your abdomen, below your stomach. It is shaped like a large tadpole, with a rounded head and slimmer, tapered body. The "head" curves into the duodenum, the first part of the small intestine. The "body" of the pancreas is located between the stomach and the spine.
The pancreas has two types of cells. Each type of cell produces a different substance as follows:
Endocrine cells produce the hormones insulin, glucagon, somatostatin and pancreatic polypeptides. Insulin helps lower blood sugar and glucagon raises blood sugar. Exocrine cells produce enzymes that help digest food in the intestines. Trypsin and chymotrypsin break down proteins. Amylase digests carbohydrates and lipase breaks down fats. 5. Conditions affecting the pancreas Diseases that may require surgery to remove the pancreas include:
Chronic pancreatitis : Inflammation in the pancreas that gets worse over time. Surgery is sometimes done to relieve pain from pancreatitis. Other pancreatic cancers and local cancers: Such as adenocarcinoma, squamous cell carcinoma, neuroendocrine tumor, intraductal papilloma, duodenal carcinoma and lymphoma. These tumors start in or near the pancreas but can spread to other parts of the body. Cancer that has spread to the pancreas from other organs may also require surgical removal of the pancreas. Pancreatic damage: If the damage is severe, you may have to have your pancreas removed. Hyperinsulinemic Hypoglycemia: This condition is caused by elevated insulin causing your blood sugar to drop very low. 6. Pancreatectomy and recovery Surgery to remove your entire pancreas is called a total pancreatectomy. Because other organs are located near your pancreas, the surgeon may also remove:
The duodenum (first part of the small intestine) Spleen Part of the stomach Gallbladder Part of the bile duct Some lymph nodes near the pancreas
You may have to drink clear water and take a laxative the day before surgery. This regimen is aimed at cleansing your bowels. You may also need to stop taking certain medications a few days before surgery, especially blood thinners such as aspirin and warfarin (Coumadin). You will be given general anesthesia during surgery to prevent pain.
After your pancreas and other organs are removed, the surgeon will reconnect your stomach and the rest of the bile duct with the second part of your intestines - the jejunum. This connection will allow food to move from your stomach into your small intestine.
If you have pancreatitis, you may have the option of an islet auto-implantation during surgery. Islet cells are cells in your pancreas that produce insulin. In autologous transplantation, the surgeon removes islet cells from the pancreas. These cells are returned to the body so that the patient can continue to produce insulin on their own.
After surgery, you will be taken to the recovery room to regain consciousness. You will have a catheter in your abdomen to drain fluid from the surgical site and a feeding catheter, which will then be removed when you can eat and drink normally.
7. Living Without a Pancreas After having surgery to remove the pancreas, you will have to make some changes to your daily lifestyle as follows:
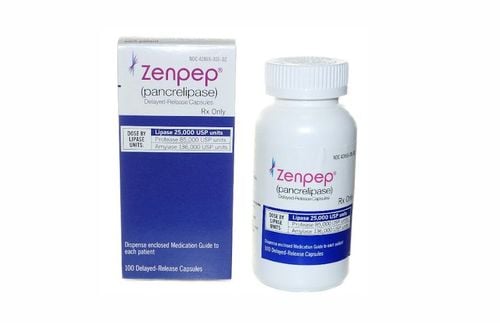
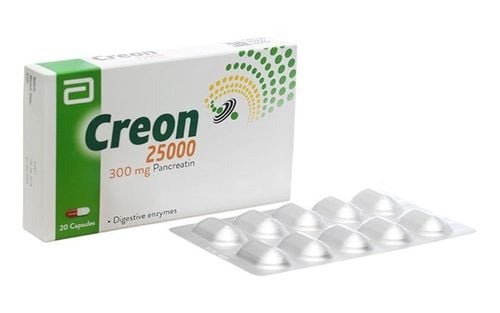
As your body will no longer produce a normal amount of insulin to control it. If you control your blood sugar, you will get diabetes. You will need to monitor your blood sugar and take insulin regularly. An endocrinologist will help you control your blood sugar. Your body also doesn't make the enzymes it needs to digest food. You will have to take an enzyme replacement pill with each meal. To stay healthy, follow a diabetic diet. You can eat a variety of foods, but watch the amount of carbohydrates and sugars in those foods. It is important to avoid low blood sugar. Try to eat several small meals throughout the day to keep your sugar levels steady. Carry glucose with you in case your blood sugar drops. Also, incorporate daily exercise. Staying active will help you regain your strength and control your blood sugar. Try walking a little bit each day to start, and ask your doctor when it's safe for you to increase the intensity of your exercise. 8. Conclusion You can live without a pancreas as well as a spleen and gallbladder, if they have also been removed. You can also live without organs such as the appendix, colon, kidneys, uterus, and ovaries (if you are a woman). However, you'll have to adjust your lifestyle, take medications your doctor prescribes and monitor your blood sugar, and stay active every day.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:Distal pancreatectomy, total pancreatectomy, and vein resection in pancreatic cancer. (2016). pancreaticcanceraction.org/about-pancreatic-cancer/treatment/operable-pancreatic-cancer/surgery-procedures-remove-tumour/ Heidt DG, et al. (2007). Total pancreatectomy: Indications, operative technique, and sequelae [Abstract]. DOI: 10.1007/s11605-006-0025-7 Islet autotransplantation for chronic pancreatitis. (n.d.). ucsfhealth.org/treatments/islet_autotransplantation_for_chronic_pancreatitis/ Muratore S, et al. (2015). Total pancreatectomy and islet auto transplantation for chronic pancreatitis. pancreapedia.org/reviews/total-pancreatectomy-and-islet-auto-transplantation-for-chronic-pancreatitis