This is an automatically translated article.
Article by Pharmacist Nguyen Thu Giang - Clinical Pharmacist - Faculty of Pharmacy - Vinmec Times City International Hospital
Tagrisso is a drug indicated to treat cancer, but the drug can cause side effects on the body. To avoid unwanted side effects, patients need to strictly follow the instructions of the doctor or pharmacist.
1. What is Tagrisso®? Tagrisso® has the active ingredient osimertinib. This is a 3rd generation epithelial growth factor receptor inhibitor (EGFR inhibitor/EGFR-TKI) indicated in metastatic non-small cell lung cancer (EGFR+). The drug was first approved by the FDA in November 2015, fully approved in 2017. In 2018, osimertinib was recommended first line for the treatment of non-small cell lung cancer with EGFR mutations. With oral tablet dosage form and once-daily dosing regimen, the drug offers hope for prolonging survival and better quality of life in patients with metastatic lung cancer.
2. Common side effects of Tagrisso ® Not all patients experience drug side effects and not all drug side effects are present in one patient. The most common side effects of Tagrisso ® include: fatigue, decreased appetite, diarrhea, severe leukopenia (including granulocytopenia, lymphocytopenia), thrombocytopenia, dry skin. , rash, nail and toenail problems such as nail color change, nail hyperpigmentation, nail breakage, nail detachment, periungitis...
You should talk to your doctor about all discomforts or unusual during the time of taking the drug, especially serious skin reactions (erythema multiforme, severe dermatitis, peeling skin necrosis...), vision changes or eye discomfort (redness of the eyes). , blurred vision, eye pain, fear of light...), respiratory symptoms (fever, cough, shortness of breath...), extreme fatigue, shortness of breath on exertion, leg or body edema.
Women should avoid becoming pregnant while taking the drug for at least 6 weeks from the last dose. Men should avoid insemination while taking the pill for at least 4 months from the last dose.
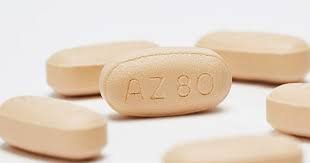
3. Can Tagrisso® affect your cardiovascular system? In clinical trials of the drug, adverse cardiovascular events of Tagrisso® were observed. Cardiomyopathy (with presenting with heart failure, congestive heart failure, pulmonary edema, or reduced ejection fraction) occurred in 1.9% of patients in the study. QTc interval prolongation >500ms on electrocardiogram occurred in 0.7% but no arrhythmias due to QTc prolongation were noted.
After the drug was placed on the market, several case reports related to heart failure and decreased cardiac function were reported. Reactions can occur days to months after taking the drug. Often, after drug discontinuation and appropriate treatment, cardiac function can return to normal in patients with early detection.
Although, the exact mechanism of cardiovascular effects of Tagrisso® is not known, it is extremely important to advise family members and patients to monitor side effects of the drug.
4. How to prevent and treat the side effects of Tagrisso ® on your cardiovascular system? Before treatment with Tagrisso®, your doctor will thoroughly evaluate and advise you and your family to monitor and prevent side effects of the drug, including side effects on the heart. circuit.
You will have an echocardiogram to evaluate your heart function (left ventricular function) before treatment and every 3 months during your treatment. You will have an electrocardiogram (electrocardiogram) before treatment and more often if you have problems such as congenital QTc prolongation, pre-existing heart failure, electrolyte disturbances, or are taking copper supplements. concomitantly with drugs that prolong the QT interval.
In the Tagrisso clinical trials, patients with a QTc interval >470ms were excluded from the study. Therefore, doctors will be more cautious and advise you more thoroughly if you have similar problems. In the event that your QTc interval increases while taking the drug, your doctor may talk to you to stop the drug for a short time and restart it at a lower dose.
Follow the treatment prescribed by the doctor, do not arbitrarily stop the drug or change the dose, because the side effects of the drug may be related to the dose of the drug used. Regular or scheduled follow-up visits for monitoring and evaluation is the best way to prevent drug side effects.
If you experience chest pain or tightness, shortness of breath (including difficulty breathing when lying down, waking up at night with a dry cough, shortness of breath, or difficulty breathing when walking or exercising), swelling in your legs or body, you need to go to the hospital for timely examination, advice and treatment.
Usually, in case your heart function is reduced on ultrasound for more than 1 month without symptoms or heart failure symptoms, Tagrisso® will be stopped and replaced with another drug. At the same time, you will be treated according to the heart failure protocol and actively monitored by a specialist.

5. Other cancer drugs that may adversely affect the cardiovascular system Anthracycline and similar drugs (eg, doxorubicin, daunorubicin, idarubicin, epirubicin, mitoxantrone) are known to pose a risk. cardiotoxicity. Drugs in this class may affect cardiac function through the formation of free radicals, oxidative stress, programmed cell death, and DNA damage by affecting enzymes and inhibiting synthesis. protein synthesis.
Risk factors that make patients more susceptible to cardiovascular toxicity due to these drugs include advanced age (>65 years old), very young age (<4 years old), female sex, decreased cardiac function from Prior, hypertension, dyslipidemia, diabetes, obesity, smoking, use of high-dose anthracycline drugs or in combination with radiation therapy or other cardiotoxic drugs.
Cardiac side effects of this class of drugs can occur within the course of treatment, then months or even years after treatment. Manifestations of side effects may include electrocardiographic abnormalities, arrhythmias, myocarditis, pericarditis, impaired cardiac function, or heart failure.
Trastuzumab often causes asymptomatic reduction in cardiac function, symptomatic heart failure is less common. The mechanism of cardiotoxicity is not fully understood, but may be related to the effect of epithelial growth factor 2 (HER2) receptor.
Other drugs: A number of cardiovascular adverse events have been observed with treatment with other cancer drugs such as cardiac arrhythmias (related to nilotinib, asciminib, ponatinib, vandetanib, crizotinib, vemurafenib, taxanes) ...); dilated cardiomyopathy, heart failure due to myocardial cell necrosis (related to sunitinib, alemtuzumab, imatinib, trametinib, taxanes... in some special subjects or in combination with other cardiotoxic drugs); prolongation of the QTc interval (related to eribulin, vandetanib...); pericarditis (associated with cytarabine, bleomycin); pericardial effusion (related to trans retinoic acid); heart failure, myocardial ischemia, cardiac arrest (related to mobocertinib, asciminib, interleukin 2...).
Usually, the cardiac side effects caused by cancer drugs can be completely or almost completely reversed with basic treatment regimens. Your doctor will advise and choose the right treatment plan for you. Before using the drug, the doctor will evaluate the overall condition, perform laboratory tests and investigations to ensure the safest.
To minimize the cardiovascular side effects of cancer drugs, optimize existing cardiovascular risk control, ensure a healthy diet, reduce alcohol and quit smoking, control Optimizing blood pressure, blood sugar and blood fat along with a moderate exercise regimen is extremely important. Adhering to treatment, discussing with your doctor all abnormalities during treatment, and scheduled follow-up visits will help you receive effective and safe treatment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.