This is an automatically translated article.
Posted by Doctor Nguyen Thi Hoai Nam - Department of Surgical Anesthesia, Vinmec Central Park International Hospital
The content of the article discusses the influence of pain, the role of cyclo-oxygenase (COX) inhibitors and prostaglandins in immunomodulation and tumor growth promotion as well as regional anesthesia in recurrence and metastasis. cancer.
1. Effect of pain
The effects of inadequately controlled pain on stress response should be considered if future regimens seek to limit perioperative opioids. Opioid analgesia and spinal bupivicaine significantly reduced postoperative LTR compared with no analgesia in live animal breast cancer, demonstrating that effective postoperative analgesia may play a role in facilitating resistance to metastasis. apartment.
2. The role of cyclo-oxygenase (COX) inhibitors and prostaglandins in immune regulation and tumor growth promotion

Kết hợp thuốc aspirin và ibuprofen làm giảm nguy cơ phát triển ung thư vú
Given this trend, it makes sense that inhibition of PG synthesis using COX inhibitors could reduce cancer progression. Epidemiological evidence suggests that long-term use of COX inhibitors reduces the risk of cancer, especially breast, colon, lung, and prostate cancers. The standard daily dose of celecoxib, a selective COX-2 inhibitor, was associated with a 69% reduction in risk in a colorectal cancer case study.
A recent cohort study of more than 2.5 million patient-years of follow-up over 10 years demonstrates that the use of any COX inhibitor is associated with a 20% reduction in colorectal cancer risk. COX-2 is often overexpressed in breast cancer, and PGE2 is thought to contribute to its metastatic potential. A meta-analysis of the effects of aspirin and ibuprofen in >520 000 patients demonstrated an association with a reduced risk of developing breast cancer. However, prolonged use of COX-2 inhibitors in particular can cause cardiovascular disease. In the absence of prospective, randomized trials, it is not possible to state whether perioperative COX inhibition can affect cancer recurrence rates.
3. Regional anesthesia
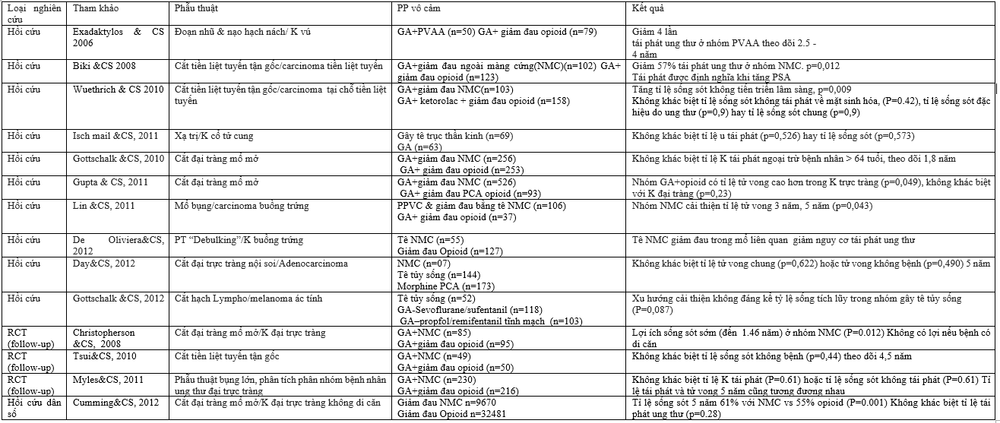
Tóm tắt các bằng chứng lâm sàng hồi cứu về tác dụng của gây tê vùng và tái phát ung thư.
Regional anesthesia reduces the neuroendocrine stress response, reducing the need for opioids and volatile anesthetics during surgery. This combination of effects may allow for enhanced preservation of perioperative immune function and may reduce the incidence of cancer recurrence. Combining spinal anesthesia with general anesthesia (GA) reduces postoperative pulmonary metastases compared with GA alone. Another study showed similar results that spinal anesthesia was associated with preservation of NK cell function in vitro. However, a recent meta-analysis showed no association between regional anesthesia and preservation of postoperative NK T-lymphocyte function compared with GA.
Small prospective clinical study of randomized breast cancer surgery patients under GA with Propofol combined with paravertebral anesthesia and continuous analgesia (PVA), or GA with sevoflurane and opioid analgesia. While propofol with PVA consistently decreased the stress response, no difference was observed in VEGF and PGE2 concentrations. But the serum of patients randomly anesthetized with propofol - PVA, as a putative "anti-cancer" anesthetic showed a greater inhibitory effect on estrogen-receptor negative breast cancer cell function compared with with serum from patients receiving standard GA.
A long-term follow-up analysis of the MASTER trial, a multicenter prospective clinical study in which major abdominal surgery patients were randomized to GA with epidural or opioid analgesia, found no improvement differences in cancer-free survival between groups. The median time to cancer recurrence or death was 2.6 years in the epidural group compared with 2.8 years in the opioid group. This is the first long-term follow-up of a patient prospectively randomly assigned to opioid analgesia or an epidural. A potential confounding factor could be the amount of volatile anesthetic required for surgery, which was not recorded in the initial MASTER trial. While the study had a strong ability to detect a one-third reduction in risk, smaller but clinically significant effects may have been overlooked. Note that older age, female sex, lymph node metastasis, and allogeneic red blood cell transfusions are all associated with reduced cancer-free survival.